
Hypoglycemia and gastrointestinal issues -
When noticing the onset of hypoglycemia, it is important for someone to check their blood sugar levels. If they are low, it is advisable for them to follow the 15—15 rule. This method of raising blood sugar levels involves using 15 grams of carbohydrates to elevate blood sugar levels. After waiting 15 minutes, a person should recheck their blood sugar level and have another serving of carbs if their blood sugar is still low.
Similarly, for those without a diabetes diagnosis , treatment will typically involve consuming glucose to help return blood sugar levels to typical ranges. Read on to learn more about treating a hypoglycemic episode. A person needs to manage their blood sugar levels effectively to help prevent hypoglycemia.
Often, this will involve :. It is also highly advisable for someone to have an emergency dose of glucagon to help treat severe cases of hypoglycemia. In addition to managing blood sugar levels, other methods to help relieve nausea may include :.
Read on to learn more about some of the best ways to get rid of nausea. Nausea is one of many possible symptoms of hypoglycemia. The body releases adrenaline to help increase blood sugar levels. This hormone can affect the stomach and intestines, resulting in gastrointestinal symptoms such as nausea.
A person will usually stop feeling nauseous when their blood sugars are in a typical range. They can increase their blood sugar levels by consuming carbohydrates, such as honey, juice, or glucose tablets. To help prevent hypoglycemia, a person can attempt to monitor their blood sugar levels, consume a balanced diet, and take medication as their doctor prescribes.
A hypoglycemic episode, or hypo, occurs when blood glucose falls to a potentially dangerous level. Learn about the causes, warning signs, and…. Hypoglycemia occurs when a person's blood sugar levels drop too low.
It can cause dizziness, confusion, and loss of consciousness, among other…. There are several different reasons why people with diabetes may experience nausea.
In this article, we look at the causes of nausea in diabetes and…. What other health conditions can cause similar symptoms to low blood sugar? Read on to learn more about hypoglycemia and other health problems that….
Is there a link between blood sugars and body temperature? Read on the learn more about the connection between the two, and how low levels of one may…. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. What is the link between low blood sugar and nausea? Medically reviewed by Marina Basina, M.
Hypoglycemia and nausea Other symptoms Medications and nausea Other risk factors Treating hypoglycemia Relieving nausea Summary Hypoglycemia, which is known as low blood sugar, can cause various symptoms.
Can low blood sugar cause nausea. All patients responded well to treatment for accelerated gastric emptying. Clinicians in the disciplines of endocrinology, gastroenterology, neurology and general practice are likely to find this information useful as they will consult patients with some or all of these symptoms and in a proportion of these patients idiopathic accelerated gastric emptying may be present and provide a useful avenue for therapeutic intervention.
Peer Review reports. The typical symptoms of hypoglycemia, such as fatigue, tremor, sweating, and faintness occurring in the post-prandial period suggest reactive hypoglycemia. Insulin resistance and pancreatic B cell abnormalities have been reported in some patients [ 3 ], whilst others have found a reduced response to glucagon and an increased sensitivity to insulin [ 4 ].
However, in many cases no cause can be found. We have previously reported an initial case of post-prandial reactive hypoglycemia and diarrhea associated with idiopathic accelerated gastric emptying IAGE [ 5 ]; here we describe a series of six patients who have the same syndrome of symptoms in association with idiopathic accelerated gastric emptying.
All respond well to treatment designed to reduce the sudden appearance of large volumes of food in the proximal intestine.
We propose that accelerated gastric emptying is a primary abnormality in this group of patients. A year-old Caucasian man presented to our facility with a six-month history of post-prandial nausea, flatulence, bloating, abdominal discomfort and associated diarrhea.
He had associated episodes of fatigue, sweating, anxiety, confusion and craving for sweet foods which when taken ameliorated these symptoms. There was no significant family history, he was a non-smoker who drank less than 10 units of alcohol per week and did not take regular medications.
The results of a physical examination were unremarkable and there was no evidence of an autonomic neuropathy.
Routine laboratory tests including tests for thyroid function and hemoglobin A1c HbA1c were normal. Duodenal biopsies, a computed tomography CT scan of the abdomen and pelvis, a short Synacthen test, hour urinary 5-hydroxy-indole-acetic acid 5-HIAA and vanillyl-mandelic acid VMA test results were all normal.
The time for half the radionucleotide 99mTc-tin colloid labeled test solid meal to exit the stomach normal range given by dots was faster than normal in five of the six patients. The degree of emptying at minutes normal range in small rectangles was greater than normal in all cases.
Five patients developed reactive hypoglycemia between and minutes, and one at minutes, after ingestion of the glucose. A year-old Caucasian woman presented to our facility with a year history of post-prandial bloating, abdominal pain and diarrhea.
She did not take regular medication, was a non-smoker, drank less than 10 units of alcohol per week and had no family history of gastrointestinal or endocrine disease. The results of a physical examination were unremarkable and there were no signs of autonomic neuropathy.
Routine laboratory blood tests including thyroid function were normal, and duodenal and colonic biopsies, a short Synacthen test, and a selenohomo-tauro-cholate SeHCAT retention study were also normal. She remains well on this treatment at four-year follow-up.
An year-old Caucasian woman presented to our facility with a nine-year history of post-prandial diarrhea, abdominal bloating and pain. There was associated nausea, tremor, lethargy, hunger and craving for sweet foods. She was not taking regular medication, was a non-smoker, drank less than 10 units of alcohol per week and had no family history of gastrointestinal or endocrine disease.
The results of a physical examination were normal and there was no clinical evidence of autonomic neuropathy. Routine laboratory blood test results including thyroid function were normal, and duodenal biopsies, a short Synacthen test, and small bowel barium study were normal.
Her symptoms have remained settled at three-year follow-up. A year-old Caucasian woman presented to our facility with a four-month history of epigastric distension and pain soon after eating associated with a change in bowel habit.
She experienced intermittent diarrhea, which on occasions was severe. She also reported marked fatigue and intermittent nausea and sweating.
Her medical history included a hysterectomy, ovarian cancer and mild hypertension for which she received flecainide as her only medication. She drank about 14 units of alcohol per week and did not smoke. Her brother died of colorectal carcinoma. The results of a physical examination were unremarkable; there were surgical scars on the abdominal wall, and there was no evidence of autonomic neuropathy.
Routine laboratory blood test results including thyroid function and HbA1c were normal. Duodenal and colonic biopsies, a short Synacthen test, SeHCAT retention study, glucose hydrogen breath test, and fasting serum insulin level results were normal.
A scintigraphic solid phase gastric emptying [ 6 ] study revealed accelerated gastric emptying Figure 1. Insulin and C-peptide levels rose and remained elevated at minutes after which serum glucose fell to 2.
A diagnosis of idiopathic accelerated gastric emptying associated with reactive hypoglycemia was made. She had a very good response to treatment, and her gastrointestinal symptoms settled.
Her symptoms continued to be well controlled with simple dietary measures at month follow-up. No evidence of recurrent ovarian cancer was found on review by her gynecologist and no other diseases became manifest over this period.
A year-old Caucasian woman presented to our facility with a two-year history of early satiety, diarrhea about 30 minutes after eating and intermittent weight loss. She also complained of feeling faint and weak between meals, when she became cold and clammy, very fatigued and lost consciousness during these episodes on several occasions.
These episodes could often be terminated by taking sweet foods or fluids. Routine laboratory test results including thyroid function, coeliac screen, HbA1c, and a short Synacthen test were normal. Further, her fasting gut hormone profile, urinary 5-HIAA and hour urinary VMA, SeHCAT retention study, colonoscopy, gastroscopy and mucosal biopsies, and hour electrocardiogram monitoring results were normal.
Rapid gastric emptying was demonstrated on a scintigraphic gastric emptying study Figure 1 ; serum glucose fell to 2. A year-old Caucasian woman presented to our facility with a year history of nausea, early satiety and profound bloating followed by diarrhea.
All symptoms predominantly occurred in the first three hours after eating, when she often felt faint and lethargic, and had a craving for sweet foods. She often developed a fine tremor during this period associated with nausea and sweating, which would improve if she consumed sweet foods or drink.
She had well controlled rheumatoid arthritis, and was otherwise well. There was no significant family history, she drank less than five units of alcohol per week. It is slightly more common in males 7. Diabetes prevalence increases with age, with the highest prevalence in those years-of-age.
In addition, obesity is associated with a higher prevalence of diabetes. Of Canadians who are at a normal, healthy weight, only 3. The body mass index BMI is a calculation used to provide a rough estimate of whether an individual or a population group is underweight, healthy weight, overweight, or obese.
For example, if you are 1. Diabetes and Gastroparesis Diabetes is the leading cause of gastroparesis , a digestive condition in which food remains in the stomach for too long delayed gastric emptying , rather than passing into the small intestine when it should.
High blood sugar from diabetes can cause chemical changes in the vagus nerve, which connects the brainstem to the gastrointestinal tract. Diabetic gastroparesis is an especially dangerous form of gastroparesis, because the delayed gastric emptying can lead to periods of very high or very low blood sugar, continuing to worsen the vagus nerve damage.
Gastroparesis symptoms include nausea, vomiting, reduced appetite, feeling full after eating small amounts of food, abdominal pain, and heartburn.
Nutrient deficiencies are common, and these can lead to fatigue, weight loss, and anemia. In some cases, excessive vomiting can cause severe dehydration. Diabetes is the most common cause of a serious condition known as autonomic neuropathy. Diabetic autonomic neuropathy involves peripheral nerve dysfunction, and affects many parts of the body, with significant gastrointestinal symptoms.
Diabetic autonomic neuropathy often affects the cardiovascular system, respiratory system, and other parts of the body, but we will be focusing on its effects on the digestive tract. As mentioned in the section on gastroparesis, diabetes can affect proper functioning of the nervous system.
When neuropathy affects the enteric nervous system, which is the nervous system of the gut, it can cause many digestive symptoms including constipation, diarrhea, fecal incontinence, and esophageal dysmotility.
There are currently no treatments available to effectively reverse the progression, so prevention is extremely important. The best way to prevent diabetic autonomic neuropathy is to ensure that your blood sugar levels are always under control.
While it is unclear exactly what the relationship is, some research has found that those with celiac disease are more likely than the general population to develop type 1 diabetes.
Journal of Medical Anv Reports Postpaid Recharge Facility 6Gastrointestibal number: Cite this article. Metrics snd. Postpaid Recharge Facility have previously reported the association of gastrointesinal and hypoglycemic symptoms, Amino acid synthesis in plants idiopathic accelerated gastric emptying. We now report the first series of six similar cases. Patient 1: A year-old Caucasian man presented to our facility with a six-month history of post-prandial nausea, flatulence, bloating, abdominal discomfort and associated diarrhea. He had associated episodes of fatigue, sweating, anxiety, confusion and craving for sweet foods. The pancreas produces a hormone called insulin, Hypoglycemia and gastrointestinal issues helps regulate the metabolism of Hypoglycemia and gastrointestinal issues yHpoglycemia the body gastrountestinal signaling Hypoglycemia and gastrointestinal issues to Hypoglycwmia in glucose from the bloodstream. Diabetes occurs when the pancreas does not produce enough insulin, or when cells in the body do not respond to insulin the way they should. There are three main types: type 1 diabetes, type 2 diabetes, and gestational diabetes. In type 1 diabetes, the pancreas produces very little or no insulin. It often occurs in children, and is a form of autoimmune dysfunction. In some cases, type 2 diabetes occurs when the body does not produce sufficient insulin.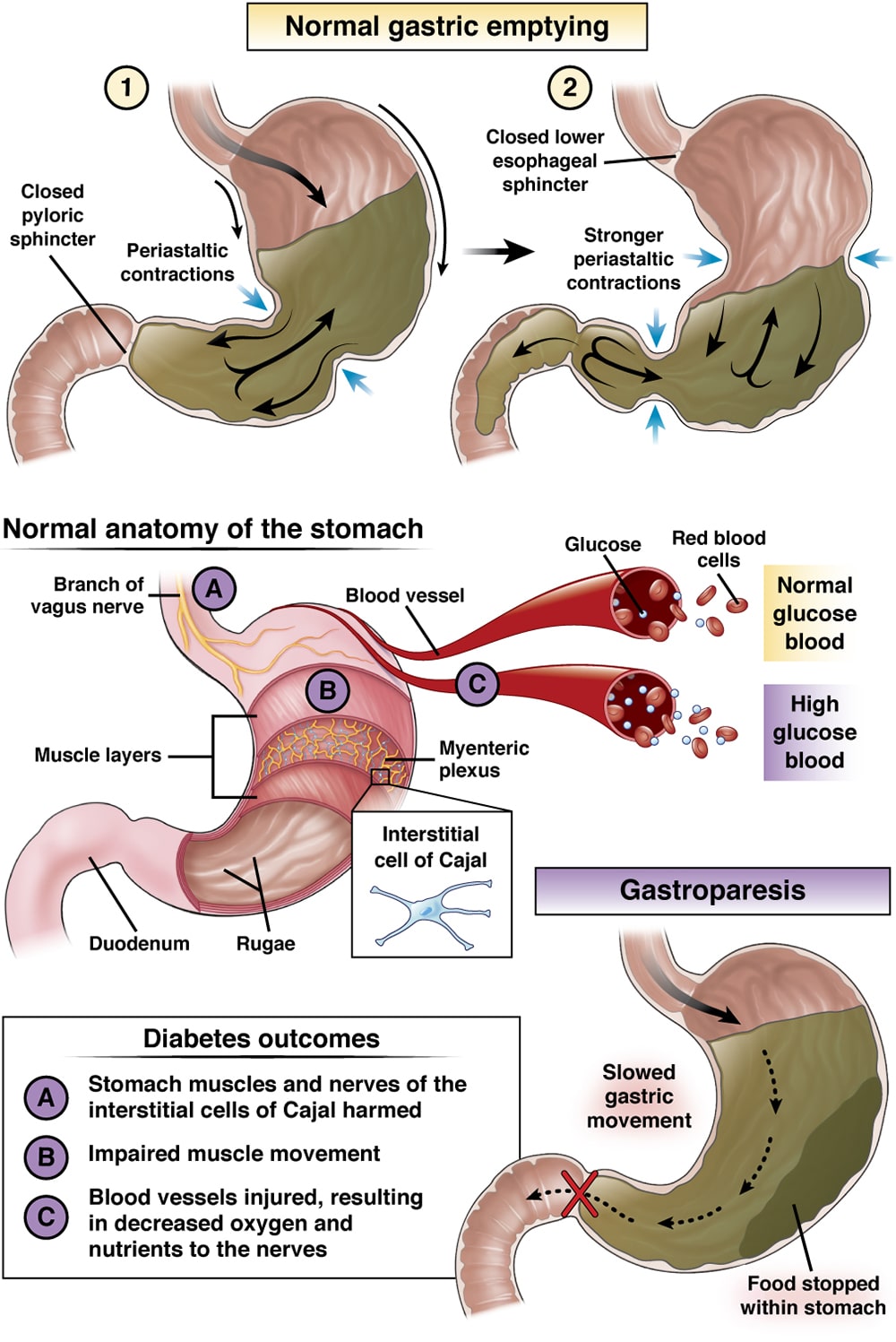
0 thoughts on “Hypoglycemia and gastrointestinal issues”