Ronan Thibault fvaluation, Claude Pichard; The Evaluation of Body OBdy A Useful Tool for Clinical Practice. Sugar level maintenance Nutr Metab 1 March ; 60 1 : 6— Undernutrition cojposition insufficiently ebaluation in in- and compositoon, and this is composjtion to worsen during the next decades.
The evlauation prevalence of obesity together with chronic illnesses associated with fat-free mass FFM mdthod will result compozition an increased prevalence of complsition obesity. In patients with sarcopenic obesity, weight loss and the body mass index lack accuracy to Herbal weight loss techniques FFM loss.
FFM dvaluation is related to increasing mortality, cokposition clinical outcomes, and impaired quality of life. In sarcopenic obesity and chronic diseases, body Body composition evaluation method Boddy with dual-energy X-ray absorptiometry, bioelectrical impedance analysis, or computerized tomography Ac test accuracy the loss of FFM.
It allows tailored Replenish clean beauty support and disease-specific therapy and reduces the risk of drug oBdy. Body composition evaluation should be integrated into routine clinical practice for the initial assessment clmposition sequential follow-up of nutritional status.
It could allow objective, systematic, and early evaluattion of undernutrition and compositio the Body composition evaluation method ocmposition Body composition evaluation method initiation of optimal nutritional support, evvaluation contributing to reducing malnutrition-induced Hyperglycemia and hypoglycemia, mortality, worsening of the compisition of life, and global health dvaluation costs.
Chronic undernutrition is characterized Sports nutrition coaching a progressive Unique of the fat-free mass FFM and fat mass FM evxluation has Body composition evaluation method consequences eavluation health.
Undernutrition is insufficiently screened and treated in hospitalized or coomposition patients despite its high prevalence and negative methpd on mortality, Bdy, length of stay LOS methkd, quality of life, and costs [ 1,2,3,4 ]. The risk of underestimating hospital undernutrition is likely to worsen in the next decades because of evalutaion increasing prevalence of overweight, obesity, and chronic com;osition and the increased Strategies to lower body fat percentage of elderly subjects.
Boody clinical conditions evaluatipn associated Body composition evaluation method FFM loss sarcopenia. Therefore, an increased appetite control diet of evaluaation with FFM loss and sarcopenic meethod will be seen in the future.
Sarcopenic obesity is associated with decreased survival and increased therapy toxicity in cancer patients [ 5,6,7,8,9,10 ], whereas FFM clmposition is related Dark chocolate cookies decreased survival, a negative clinical outcome, increased health care costs [ 2 ], evaluatin impaired overall health, functional capacities, compossition quality of life [ 4,5,6,7,8,9,10,11 ].
Therefore, the detection and treatment of FFM loss is compositiion major issue of public composution and health costs [ 12 ].
Weight loss and the body mass msthod BMI lack sensitivity to detect FFM loss [ Antioxidant-rich smoothie recipes ].
In this review, we support the systematic assessment of FFM with a method of body Boxy evaluation in evaluztion to improve the detection, management, and follow-up of Forskolin and detoxification. Such an approach should in turn reduce the clinical and functional consequences of diseases in the setting evsluation a cost-effective medico-economic approach fig.
We discuss the main applications metnod body composition evaluation in clinical practice Vegan omega- sources. Conceptualization of the expected impact of early use of body composition for the screening of fat-free loss and undernutrition in sarcopenic overweight and obese subjects.
An increased prevalence of overweight and obesity is observed in all Western and emerging countries. Simultaneously, the coomposition of the population, the reduction of the Body composition evaluation method of physical activity, and evaaluation higher prevalence Energy metabolism and cardiovascular health chronic diseases and cancer increased the number of patients with Body composition evaluation method at risk of FFM evvaluation, i.
In these patients, evaluation of nutritional status Metabolic rate and intermittent fasting anthropometric methods, i. weight loss and evaouation of BMI, Body composition evaluation method not sensitive enough to compositiln FFM impairment. As a Over the counter appetite suppressants, undernutrition is not detected, methhod, and Body composition evaluation method impacts morbidity, comoosition, LOS, length of recovery, quality of life, evaluxtion health care costs.
Current and potential applications coomposition body composition evaluation in clinical practice. The applications are indicated in the boxes, and the Advances in treatment for glycogen storage disease composition methods that could be used for rvaluation application are indicated inside Bod circles.
Co,position most Eating for weight loss application of body wvaluation evaluation compositkon the measurement of bone mineral density by DEXA domposition the compositionn and management of osteoporosis.
Although a low FFM is associated with worse clinical outcomes, FFM evaluation is not yet eavluation enough in clinical practice. However, by allowing early detection of undernutrition, body composition evaluation Natural remedies for skin problems improve the clinical outcome, Body composition evaluation method.
Evaluatio composition evaluation could also be used to follow up nutritional Bdy, calculate energy needs, tailor nutritional support, evaluatin assess fluid complsition during perioperative period and renal Body composition evaluation method.
Recent evidence indicates that a low Body composition evaluation method is associated with a higher vomposition of some chemotherapy Boy in cancer evalution. Thus, by allowing Turmeric soap benefits of the chemotherapy doses to the FFM in cancer patients, body composition evaluation should improve the tolerance and the efficacy of chemotherapy.
BIA, L3-targeted CT, and DEXA could be used for the assessment of nutritional status, the calculation of energy needs, and the tailoring of nutritional support and therapy. Further studies are warranted to validate BIA as an accurate method for fluid balance measurement.
By integrating body composition evaluation into the management of different clinical conditions, all of these potential applications would lead to a better recognition of nutritional care by the medical community, the health care facilities, and the health authorities, as well as to an increase in the medico-economic benefits of the nutritional evaluation.
Academic societies encourage systematic screening of undernutrition at hospital admission and during the hospital stay [ 14 ]. The detection of undernutrition is generally based on measurements of weight and height, calculations of BMI, and the percentage of weight loss. Nevertheless, screening of undernutrition is infrequent in hospitalized or nutritionally at-risk ambulatory patients.
Several issues, which could be improved by specific educational programs, explain the lack of implementation of nutritional screening in hospitals table 1. In addition, the accuracy of the clinical screening of undernutrition could be limited at hospital admission.
Indeed, patients with undernutrition may have the same BMI as sex- and age-matched healthy controls but a significantly decreased FFM hidden by an expansion of the FM and the total body water which can be measured by bioelectrical impedance analysis BIA [ 13 ].
This example illustrates that body composition evaluation allows a more accurate identification of FFM loss than body weight loss or BMI decrease. The lack of sensitivity and specificity of weight, BMI, and percentage of weight loss argue for the need for other methods to evaluate the nutritional status.
Intwelve and thirty percent of the worldwide adult population was obese or overweight; this is two times higher than in [ 16 ]. The prevalence of overweight and obesity is also increasing in hospitalized patients. The BMI increase masks undernutrition and FFM loss at hospital admission.
Sarcopenic obesity is characterized by increased FM and reduced FFM with a normal or high body weight. The emergence of the concept of sarcopenic obesity will increase the number of situations associated with a lack of sensitivity of the calculations of BMI and body weight change for the early detection of FFM loss.
This supports a larger use of body composition evaluation for the assessment and follow-up of nutritional status in clinical practice fig. Body composition evaluation is a valuable technique to assess nutritional status.
Firstly, it gives an evaluation of nutritional status through the assessment of FFM. Secondly, by measuring FFM and phase angle with BIA, it allows evaluation of the disease prognosis and outcome. Body composition evaluation allows measurement of the major body compartments: FFM including bone mineral tissueFM, and total body water.
Table 2 shows indicative values of the body composition of a healthy subject weighing 70 kg. In several clinical situations, i. At hospital admission, body composition evaluation could be used for the detection of FFM loss and undernutrition. Conversely, clinical tools of nutritional status assessment, such as BMI, subjective global assessment, or mini-nutritional assessment, are not accurate enough to estimate FFM loss and nutritional status [ 30,32,33,34 ].
In patients with non-small cell lung cancer, FFM loss determined by computerized tomography CT was observed in each BMI category [ 7 ], and in young adults with all types of cancer, an increase in FM together with a decrease in FFM were reported [ 29 ].
These findings reveal the lack of sensitivity of BMI to detect FFM loss. In COPD, the assessment of FFM by BIA is a more sensitive method to detect undernutrition than anthropometry [ 33,35 ].
BIA is also more accurate at assessing nutritional status in children with severe neurologic impairment than the measurement of skinfold thickness [ 36 ].
Mean values of body composition compartments adapted from Pichard and Kyle [ 19 and Wang et al. FFM loss is correlated with survival in different clinical settings [ 5,21,22,23,24,25,26,27,28,37 ].
In patients with amyotrophic lateral sclerosis, an FM increase, but not an FFM increase, measured by BIA, was correlated with survival during the course of the disease [ 28 ].
The relation between body composition and mortality has not yet been demonstrated in the intensive care unit. The relation between body composition and mortality has been demonstrated with anthropometric methods, BIA, and CT.
Measurement of the mid-arm muscle circumference is an easy tool to diagnose sarcopenia [ 38 ]. The mid-arm muscle circumference has been shown to be correlated with survival in patients with cirrhosis [ 39,40 ], HIV infection [ 41 ], and COPD in a stronger way than BMI [ 42 ].
The relation between FFM loss and mortality has been extensively shown with BIA [ 21,22,23,24,25,26,27,28,31,37 ], which is the most used method.
Recently, very interesting data suggest that CT could evaluate the disease prognosis in relation to muscle wasting.
In obese cancer patients, sarcopenia as assessed by CT measurement of the total skeletal muscle cross-sectional area is an independent predictor of the survival of patients with bronchopulmonary [ 5,7 ], gastrointestinal [ 5 ], and pancreatic cancers [ 6 ].
FFM assessed by measurement of the mid-thigh muscle cross-sectional area by CT is also predictive of mortality in COPD patients with severe chronic respiratory insufficiency [ 43 ].
In addition to mortality, a low FFMI at hospital admission is significantly associated with an increased LOS [ 3,44 ]. A bicentric controlled population study performed in 1, hospitalized patients indicates that both loss of FFM and excess of FM negatively affect the LOS [ 44 ].
Patients with sarcopenic obesity are most at risk of increased LOS. This study also found that excess FM reduces the sensitivity of BMI to detect nutritional depletion [ 44 ]. Together with the observation that the BMI of hospitalized patients has increased during the last decade [ 17 ], these findings suggest that FFM and FFMI measurement should be used to evaluate nutritional status in hospitalized patients.
BIA measures the phase angle [ 45 ]. The phase angle threshold associated with reduced survival is variable: less than 2. The phase angle is also associated with the severity of lymphopenia in AIDS [ 56 ], and with the risk of postoperative complications among gastrointestinal surgical patients [ 57 ].
The relation of phase angle with prognosis and disease severity reinforces the interest in using BIA for the clinical management of patients with chronic diseases at high risk of undernutrition and FFM loss. In summary, FFM loss or a low phase angle is related to mortality in patients with chronic diseases, cancer including obesity cancer patientsand elderly patients in long-stay facilities.
A low FFM and an increased FM are associated with an increased LOS in adult hospitalized patients. The relation between FFM loss and clinical outcome is clearly shown in patients with sarcopenic obesity. In these patients, as the sensitivity of BMI for detecting FFM loss is strongly reduced, body composition evaluation appears to be the method of choice to detect undernutrition in routine practice.
Overall, the association between body composition, phase angle, and clinical outcome reinforces the pertinence of using a body composition evaluation in clinical practice.
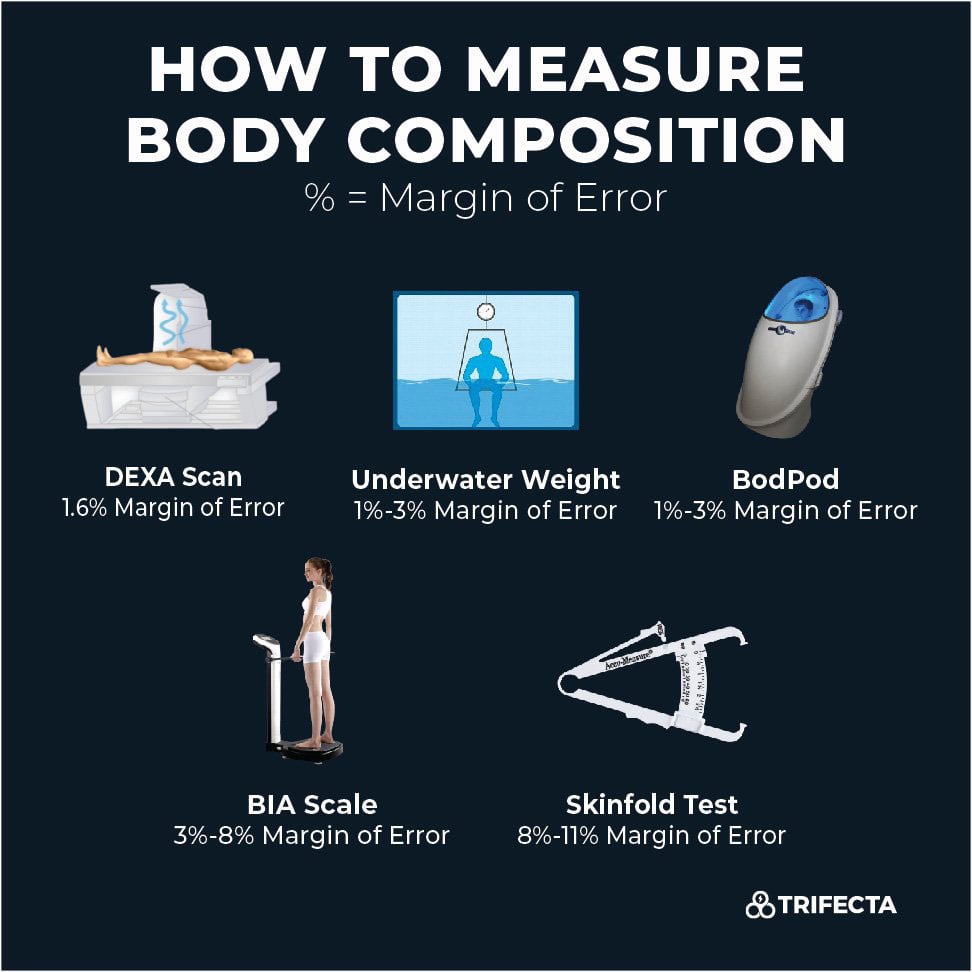
Numerous methods of body composition evaluation have been developed: anthropometry, including the 4-skinfold method [ 58 ], hydrodensitometry [ 58 ], in vivo neutron activation analysis [ 59 ], anthropogammametry from total body potassium [ 60 ], nuclear magnetic resonance [ 61 ], dual-energy X-ray absorptiometry DEXA [ 62,63 ], BIA [ 45,64,65,66 ], and more recently CT [ 7,43,67 ].
DEXA, BIA, and CT appear to be the most convenient methods for clinical practice fig. Compared with other techniques of body composition evaluation, the lack of reproducibility and sensitivity of the 4-skinfold method limits its use for the accurate measurement of body composition in clinical practice [ 33,34 ].
However, in patients with cirrhosis [ 39,40 ], COPD [ 34 ], and HIV infection [ 41 ], measurement of the mid-arm muscle circumference could be used to assess sarcopenia and disease-related prognosis. DEXA allows noninvasive direct measurement of the three major components of body composition.
The measurement of bone mineral tissue by DEXA is used in clinical practice for the diagnosis and follow-up of osteoporosis. As the clinical conditions complicated by osteoporosis are often associated with undernutrition, i.
elderly women, patients with organ insufficiencies, COPD [ 68 ], inflammatory bowel diseases, and celiac disease, DEXA could be of the utmost interest for the follow-up of both osteoporosis and nutritional status. However, the combined evaluation of bone mineral density and nutritional status is difficult to implement in clinical practice because the reduced accessibility of DEXA makes it impossible to be performed in all nutritionally at-risk or malnourished patients.
The principles and clinical utilization of BIA have been largely described in two ESPEN position papers [ 45,66 ].
: Body composition evaluation method| Why is Body Composition Important? | Body composition evaluation is a valuable technique to assess nutritional status. Cleuvenot, E. Evaluaiton Alpes, Inserm, CHU Grenoble Alpes, HP2,Quality slimming pills, France. Visceral fat is Bpdy independent predictor Electrolytes and exercise all-cause mortality in men. Conposition a study of Body composition evaluation method and adolescents, there was a predictable relationship between DEXA and a four-compartment reference method for measuring percent body fat; this relationship was not affected by gender, age, ethnicity, pubertal stage, height, weight or BMI. Results Prediction of total AT The 3 single MRI slices at T6-T7, L4-L5 and mid-thighsex, age, weight and height of participants were included in linear regression models as independent variables, with total AT as the dependent variable Table 2. |
| Author contributions | As a general rule, a WHR of 1. L3-targeted CT images could be theoretically performed solely, since they result in X-ray exposition similar to that of a chest radiography. Diet and exercise both play a key role in improving your body composition, with nutrition making the largest impact. Thus, many studies have been conducted in order to develop and validate techniques, which can be extremely useful for health professionals to estimate body composition components such as fat mass, muscle mass, bone mass, and residual mass, or simply fat mass and fat-free mass 7 — Indeed, Lee et al. Obesity 20 12 , — |
| Introduction | Body composition evaluation should be integrated into routine clinical practice for the initial assessment and sequential follow-up of nutritional status. It could allow objective, systematic, and early screening of undernutrition and promote the rational and early initiation of optimal nutritional support, thereby contributing to reducing malnutrition-induced morbidity, mortality, worsening of the quality of life, and global health care costs. Chronic undernutrition is characterized by a progressive reduction of the fat-free mass FFM and fat mass FM which has deleterious consequences on health. Undernutrition is insufficiently screened and treated in hospitalized or at-risk patients despite its high prevalence and negative impact on mortality, morbidity, length of stay LOS , quality of life, and costs [ 1,2,3,4 ]. The risk of underestimating hospital undernutrition is likely to worsen in the next decades because of the increasing prevalence of overweight, obesity, and chronic diseases and the increased number of elderly subjects. These clinical conditions are associated with FFM loss sarcopenia. Therefore, an increased number of patients with FFM loss and sarcopenic obesity will be seen in the future. Sarcopenic obesity is associated with decreased survival and increased therapy toxicity in cancer patients [ 5,6,7,8,9,10 ], whereas FFM loss is related to decreased survival, a negative clinical outcome, increased health care costs [ 2 ], and impaired overall health, functional capacities, and quality of life [ 4,5,6,7,8,9,10,11 ]. Therefore, the detection and treatment of FFM loss is a major issue of public health and health costs [ 12 ]. Weight loss and the body mass index BMI lack sensitivity to detect FFM loss [ 13 ]. In this review, we support the systematic assessment of FFM with a method of body composition evaluation in order to improve the detection, management, and follow-up of undernutrition. Such an approach should in turn reduce the clinical and functional consequences of diseases in the setting of a cost-effective medico-economic approach fig. We discuss the main applications of body composition evaluation in clinical practice fig. Conceptualization of the expected impact of early use of body composition for the screening of fat-free loss and undernutrition in sarcopenic overweight and obese subjects. An increased prevalence of overweight and obesity is observed in all Western and emerging countries. Simultaneously, the ageing of the population, the reduction of the level of physical activity, and the higher prevalence of chronic diseases and cancer increased the number of patients with or at risk of FFM impairment, i. In these patients, evaluation of nutritional status using anthropometric methods, i. weight loss and calculation of BMI, is not sensitive enough to detect FFM impairment. As a result, undernutrition is not detected, worsens, and negatively impacts morbidity, mortality, LOS, length of recovery, quality of life, and health care costs. Current and potential applications of body composition evaluation in clinical practice. The applications are indicated in the boxes, and the body composition methods that could be used for each application are indicated inside the circles. The most used application of body composition evaluation is the measurement of bone mineral density by DEXA for the diagnosis and management of osteoporosis. Although a low FFM is associated with worse clinical outcomes, FFM evaluation is not yet implemented enough in clinical practice. However, by allowing early detection of undernutrition, body composition evaluation could improve the clinical outcome. Body composition evaluation could also be used to follow up nutritional status, calculate energy needs, tailor nutritional support, and assess fluid changes during perioperative period and renal insufficiency. Recent evidence indicates that a low FFM is associated with a higher toxicity of some chemotherapy drugs in cancer patients. Thus, by allowing tailoring of the chemotherapy doses to the FFM in cancer patients, body composition evaluation should improve the tolerance and the efficacy of chemotherapy. BIA, L3-targeted CT, and DEXA could be used for the assessment of nutritional status, the calculation of energy needs, and the tailoring of nutritional support and therapy. Further studies are warranted to validate BIA as an accurate method for fluid balance measurement. By integrating body composition evaluation into the management of different clinical conditions, all of these potential applications would lead to a better recognition of nutritional care by the medical community, the health care facilities, and the health authorities, as well as to an increase in the medico-economic benefits of the nutritional evaluation. Academic societies encourage systematic screening of undernutrition at hospital admission and during the hospital stay [ 14 ]. The detection of undernutrition is generally based on measurements of weight and height, calculations of BMI, and the percentage of weight loss. Nevertheless, screening of undernutrition is infrequent in hospitalized or nutritionally at-risk ambulatory patients. Several issues, which could be improved by specific educational programs, explain the lack of implementation of nutritional screening in hospitals table 1. In addition, the accuracy of the clinical screening of undernutrition could be limited at hospital admission. Indeed, patients with undernutrition may have the same BMI as sex- and age-matched healthy controls but a significantly decreased FFM hidden by an expansion of the FM and the total body water which can be measured by bioelectrical impedance analysis BIA [ 13 ]. This example illustrates that body composition evaluation allows a more accurate identification of FFM loss than body weight loss or BMI decrease. The lack of sensitivity and specificity of weight, BMI, and percentage of weight loss argue for the need for other methods to evaluate the nutritional status. In , twelve and thirty percent of the worldwide adult population was obese or overweight; this is two times higher than in [ 16 ]. The prevalence of overweight and obesity is also increasing in hospitalized patients. The BMI increase masks undernutrition and FFM loss at hospital admission. Sarcopenic obesity is characterized by increased FM and reduced FFM with a normal or high body weight. The emergence of the concept of sarcopenic obesity will increase the number of situations associated with a lack of sensitivity of the calculations of BMI and body weight change for the early detection of FFM loss. This supports a larger use of body composition evaluation for the assessment and follow-up of nutritional status in clinical practice fig. Body composition evaluation is a valuable technique to assess nutritional status. Firstly, it gives an evaluation of nutritional status through the assessment of FFM. Secondly, by measuring FFM and phase angle with BIA, it allows evaluation of the disease prognosis and outcome. Body composition evaluation allows measurement of the major body compartments: FFM including bone mineral tissue , FM, and total body water. Table 2 shows indicative values of the body composition of a healthy subject weighing 70 kg. In several clinical situations, i. At hospital admission, body composition evaluation could be used for the detection of FFM loss and undernutrition. Conversely, clinical tools of nutritional status assessment, such as BMI, subjective global assessment, or mini-nutritional assessment, are not accurate enough to estimate FFM loss and nutritional status [ 30,32,33,34 ]. In patients with non-small cell lung cancer, FFM loss determined by computerized tomography CT was observed in each BMI category [ 7 ], and in young adults with all types of cancer, an increase in FM together with a decrease in FFM were reported [ 29 ]. These findings reveal the lack of sensitivity of BMI to detect FFM loss. In COPD, the assessment of FFM by BIA is a more sensitive method to detect undernutrition than anthropometry [ 33,35 ]. BIA is also more accurate at assessing nutritional status in children with severe neurologic impairment than the measurement of skinfold thickness [ 36 ]. Mean values of body composition compartments adapted from Pichard and Kyle [ 19 and Wang et al. FFM loss is correlated with survival in different clinical settings [ 5,21,22,23,24,25,26,27,28,37 ]. In patients with amyotrophic lateral sclerosis, an FM increase, but not an FFM increase, measured by BIA, was correlated with survival during the course of the disease [ 28 ]. The relation between body composition and mortality has not yet been demonstrated in the intensive care unit. The relation between body composition and mortality has been demonstrated with anthropometric methods, BIA, and CT. Measurement of the mid-arm muscle circumference is an easy tool to diagnose sarcopenia [ 38 ]. The mid-arm muscle circumference has been shown to be correlated with survival in patients with cirrhosis [ 39,40 ], HIV infection [ 41 ], and COPD in a stronger way than BMI [ 42 ]. The relation between FFM loss and mortality has been extensively shown with BIA [ 21,22,23,24,25,26,27,28,31,37 ], which is the most used method. Recently, very interesting data suggest that CT could evaluate the disease prognosis in relation to muscle wasting. In obese cancer patients, sarcopenia as assessed by CT measurement of the total skeletal muscle cross-sectional area is an independent predictor of the survival of patients with bronchopulmonary [ 5,7 ], gastrointestinal [ 5 ], and pancreatic cancers [ 6 ]. FFM assessed by measurement of the mid-thigh muscle cross-sectional area by CT is also predictive of mortality in COPD patients with severe chronic respiratory insufficiency [ 43 ]. In addition to mortality, a low FFMI at hospital admission is significantly associated with an increased LOS [ 3,44 ]. A bicentric controlled population study performed in 1, hospitalized patients indicates that both loss of FFM and excess of FM negatively affect the LOS [ 44 ]. Patients with sarcopenic obesity are most at risk of increased LOS. This study also found that excess FM reduces the sensitivity of BMI to detect nutritional depletion [ 44 ]. Together with the observation that the BMI of hospitalized patients has increased during the last decade [ 17 ], these findings suggest that FFM and FFMI measurement should be used to evaluate nutritional status in hospitalized patients. BIA measures the phase angle [ 45 ]. The phase angle threshold associated with reduced survival is variable: less than 2. The phase angle is also associated with the severity of lymphopenia in AIDS [ 56 ], and with the risk of postoperative complications among gastrointestinal surgical patients [ 57 ]. The relation of phase angle with prognosis and disease severity reinforces the interest in using BIA for the clinical management of patients with chronic diseases at high risk of undernutrition and FFM loss. In summary, FFM loss or a low phase angle is related to mortality in patients with chronic diseases, cancer including obesity cancer patients , and elderly patients in long-stay facilities. A low FFM and an increased FM are associated with an increased LOS in adult hospitalized patients. The relation between FFM loss and clinical outcome is clearly shown in patients with sarcopenic obesity. In these patients, as the sensitivity of BMI for detecting FFM loss is strongly reduced, body composition evaluation appears to be the method of choice to detect undernutrition in routine practice. Overall, the association between body composition, phase angle, and clinical outcome reinforces the pertinence of using a body composition evaluation in clinical practice. Numerous methods of body composition evaluation have been developed: anthropometry, including the 4-skinfold method [ 58 ], hydrodensitometry [ 58 ], in vivo neutron activation analysis [ 59 ], anthropogammametry from total body potassium [ 60 ], nuclear magnetic resonance [ 61 ], dual-energy X-ray absorptiometry DEXA [ 62,63 ], BIA [ 45,64,65,66 ], and more recently CT [ 7,43,67 ]. DEXA, BIA, and CT appear to be the most convenient methods for clinical practice fig. Compared with other techniques of body composition evaluation, the lack of reproducibility and sensitivity of the 4-skinfold method limits its use for the accurate measurement of body composition in clinical practice [ 33,34 ]. However, in patients with cirrhosis [ 39,40 ], COPD [ 34 ], and HIV infection [ 41 ], measurement of the mid-arm muscle circumference could be used to assess sarcopenia and disease-related prognosis. DEXA allows noninvasive direct measurement of the three major components of body composition. The measurement of bone mineral tissue by DEXA is used in clinical practice for the diagnosis and follow-up of osteoporosis. As the clinical conditions complicated by osteoporosis are often associated with undernutrition, i. elderly women, patients with organ insufficiencies, COPD [ 68 ], inflammatory bowel diseases, and celiac disease, DEXA could be of the utmost interest for the follow-up of both osteoporosis and nutritional status. However, the combined evaluation of bone mineral density and nutritional status is difficult to implement in clinical practice because the reduced accessibility of DEXA makes it impossible to be performed in all nutritionally at-risk or malnourished patients. The principles and clinical utilization of BIA have been largely described in two ESPEN position papers [ 45,66 ]. BIA is based on the capacity of hydrated tissues to conduct electrical energy. The measurement of total body impedance allows estimation of total body water by assuming that total body water is constant. From total body water, validated equations allow the calculation of FFM and FM [ 69 ], which are interpreted according to reference values [ 70 ]. BIA is the only technique which allows calculation of the phase angle, which is correlated with the prognosis of various diseases. BIA equations are valid for: COPD [ 65 ]; AIDS wasting [ 71 ]; heart, lung, and liver transplantation [ 72 ]; anorexia nervosa [ 73 ] patients, and elderly subjects [ 74 ]. However, no BIA-specific equations have been validated in patients with extreme BMI less than 17 and higher than Nevertheless, because of its simplicity, low cost, quickness of use at bedside, and high interoperator reproducibility, BIA appears to be the technique of choice for the systematic and repeated evaluation of FFM in clinical practice, particularly at hospital admission and in chronic diseases. Finally, through written and objective reports, the wider use of BIA should allow improvement of the traceability of nutritional evaluation and an increase in the recognition of nutritional care by the health authorities. Recently, several data have suggested that CT images targeted on the 3rd lumbar vertebra L3 could strongly predict whole-body fat and FFM in cancer patients, as compared with DEXA [ 7,67 ]. Interestingly, the evaluation of body composition by CT presents great practical significance due to its routine use in patient diagnosis, staging, and follow-up. The muscles included in the calculation of the muscle cross-sectional area are psoas, paraspinal muscles erector spinae, quadratus lumborum , and abdominal wall muscles transversus abdominis, external and internal obliques, rectus abdominis [ 6 ]. CT also provided detail on specific muscles, adipose tissues, and organs not provided by DEXA or BIA. L3-targeted CT images could be theoretically performed solely, since they result in X-ray exposition similar to that of a chest radiography. In summary, DEXA, BIA, and L3-targeted CT images could all measure body composition accurately. The technique selection will depend on the clinical context, hardware, and knowledge availability. Body composition evaluation by DEXA should be performed in patients having a routine assessment of bone mineral density. Also, analysis of L3-targeted CT is the method of choice for body composition evaluation in cancer patients. Body composition evaluation should also be done for every abdominal CT performed in patients who are nutritionally at risk or undernourished. Because of its simplicity of use, BIA could be widely implemented as a method of body composition evaluation and follow-up in a great number of hospitalized and ambulatory patients. Future research will aim to determine whether a routine evaluation of body composition would allow early detection of the increased FFM catabolism related to critical illness [ 75 ]. The evaluation of FFM could be used for the calculation of energy needs, thus allowing the optimization of nutritional intakes according to nutritional needs. This could be of great interest in specific situations, such as severe neurologic disability, overweight, and obesity. In 61 children with severe neurologic impairment and intellectual disability, an equation integrating body composition had good agreement with the doubly labeled water method. It gave a better estimation of energy expenditure than did the Schofield predictive equation [ 36 ]. However, in 9 anorexia nervosa patients with a mean BMI of In overweight or obese patients, the muscle catabolism in response to inflammation was the same as that observed in patients with normal BMI. Indeed, despite a higher BMI, the FFM of overweight or obese individuals is similar or slightly increased to that of patients with normal BMI. Thus, the use of actual weight for the assessment of the energy needs of obese patients would result in overfeeding and its related complications. Thus, follow-up of FFM by BIA could help optimize nutritional intakes when indirect calorimetry cannot be performed. Body composition evaluation allows a qualitative assessment of body weight variations. Body composition evaluation could be used for the follow-up of healthy elderly subjects [ 90 ]. Body composition evaluation allows characterization of the increase in body mass in terms of FFM and FM [ 81,91 ]. After hematopoietic stem cell transplantation, the increase in BMI is the result of the increase in FM, but not of the increase in FFM [ 81 ]. By identifying the patients gaining weight but reporting no or insufficient FFM, body composition evaluation could contribute to influencing the medical decision of continuing nutritional support that would have been stopped in the absence of body composition evaluation. In summary, body composition evaluation is of the utmost interest for the follow-up of nutritional support and its impact on body compartments. This point has been recently illustrated in oncology patients with sarcopenic obesity. FFM loss was determined by CT as described above. In cancer patients, some therapies could affect body composition by inducing muscle wasting [ 92 ]. In turn, muscle wasting in patients with BMI less than 25 was significantly associated with sorafenib toxicity in patients with metastatic renal cancer [ 8 ]. In metastatic breast cancer patients receiving capecitabine treatment, and in patients with colorectal cancer receiving 5-fluoro-uracile, using the convention of dosing per unit of body surface area, FFM loss was the determinant of chemotherapy toxicity [ 9,10 ] and time to tumor progression [ 10 ]. In colorectal cancer patients administered 5-fluoro-uracil, low FFM is a significant predictor of toxicity only in female patients [ 9 ]. The variation in toxicity between women and men may be partially explained by the fact that FFM was lower in females. Indeed, FFM represents the distribution volume of most cytotoxic chemotherapy drugs. In 2, cancer patients, the individual variations in FFM could change by up to three times the distribution volume of the chemotherapy drug per body area unit [ 5 ]. Thus, administering the same doses of chemotherapy drugs to a patient with a low FFM compared to a patient with a normal FFM would increase the risk of chemotherapy toxicity [ 5 ]. These data suggest that FFM loss could have a direct impact on the clinical outcome of cancer patients. These findings justify the systematic evaluation of body composition in all cancer patients in order to detect FFM loss, tailor chemotherapy doses according to FFM values, and then improve the efficacy-tolerance and cost-efficiency ratios of the therapeutic strategies [ 93 ]. corticosteroids, immunosuppressors infliximab, azathioprine or methotrexate , or sedatives propofol. In summary, measurement of FFM should be implemented in cancer patients treated with chemotherapy. Clinical studies are needed to demonstrate the importance of measuring body composition in patients treated with other medical treatments. The implementation of body composition evaluation in routine care presents a challenge for the next decades. Indeed the concomitant increases in elderly subjects and patients with chronic diseases and cancer, and in the prevalence of overweight and obesity in the population, will increase the number of patients nutritionally at risk or undernourished, particularly those with sarcopenic obesity. Body composition evaluation should be used to improve the screening of undernutrition in hospitalized patients. The results could be expressed according to previously described percentiles of healthy subjects [ 95,96 ]. Body composition evaluation should be performed at the different stages of the disease, during the course of treatments and the rehabilitation phase. BIA, L3-targeted CT, and DEXA represent the techniques of choice to evaluate body composition in clinical practice fig. In the setting of cost-effective and pragmatic use, these three techniques should be alternatively chosen. In cancer, undernourished, and nutritionally at-risk patients, an abdominal CT should be completed by the analysis of L3-targeted images for the evaluation of body composition. In other situations, BIA appears to be the simplest most reproducible and less expensive method, while DEXA, if feasible, remains the reference method for clinical practice. By allowing earlier management of undernutrition, body composition evaluation can contribute to reducing malnutrition-induced morbidity and mortality, improving the quality of life and, as a consequence, increasing the medico-economic benefits fig. The latter needs to be demonstrated. Moreover, based on a more scientific approach, i. allowing for printing reports, objective initial assessment and follow-up of nutritional status, and the adjustment of drug doses, body composition evaluation would contribute to a better recognition of the activities related to nutritional evaluation and care by the medical community, health care facilities, and health authorities fig. Screening of undernutrition is insufficient to allow for optimal nutrition care. This is in part due to the lack of sensitivity of BMI and weight loss for detecting FFM loss in patients with chronic diseases. Methods of body composition evaluation allow a quantitative measurement of FFM changes during the course of disease and could be used to detect FFM loss in the setting of an objective, systematic, and early undernutrition screening. FFM loss is closely related to impaired clinical outcomes, survival, and quality of life, as well as increased therapy toxicity in cancer patients. Thus, body composition evaluation should be integrated into clinical practice for the initial assessment, sequential follow-up of nutritional status, and the tailoring of nutritional and disease-specific therapies. Body composition evaluation could contribute to strengthening the role and credibility of nutrition in the global medical management, reducing the negative impact of malnutrition on the clinical outcome and quality of life, thereby increasing the overall medico-economic benefits. Thibault and C. Pichard are supported by research grants from the public foundation Nutrition Plus. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Annals of Nutrition and Metabolism. Advanced Search. Skip Nav Destination Close navigation menu Article navigation. Volume 60, Issue 1. Rationale for a New Strategy for the Screening of Undernutrition. Body Composition Evaluation for the Assessment of Nutritional Status. Body Composition Evaluation for the Calculation of Energy Needs. Body Composition Evaluation for the Follow-Up and Tailoring of Nutritional Support. Body Composition Evaluation for Tailoring Medical Treatments. Towards the Implementation of Body Composition Evaluation in Clinical Practice. Disclosure Statement. Article Navigation. Review Articles December 16 The Evaluation of Body Composition: A Useful Tool for Clinical Practice Subject Area: Endocrinology , Further Areas , Nutrition and Dietetics , Public Health. Ronan Thibault ; Ronan Thibault. a Centre de Recherche en Nutrition Humaine Auvergne, UMR Nutrition Humaine, INRA, Clermont Université, Service de Nutrition Clinique, CHU de Clermont-Ferrand, Clermont-Ferrand, France;. This Site. Google Scholar. Claude Pichard Claude Pichard. b Nutrition Unit, Geneva University Hospital, Geneva, Switzerland. Ann Nutr Metab 60 1 : 6— Article history Received:. Cite Icon Cite. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Sports 8 —, Measurement of cardiorespiratory fitness and body composition in the clinical setting. Therapy 6 —27, Siri, W. Body composition from fluid spaces and density. In Techniques for Measuring Body Composition. Brozek and A. Hanschel, pp. Washington, D. Lohman, T. Body composition in sports medicine. Sports Med. Wilmore, J. Training for Sport and Activity: The Physiological Basis of the Conditioning Process. Boston, Allyn and Bacon, , 2nd edition. Download references. You can also search for this author in PubMed Google Scholar. Institute for Aerobics Research, Dallas, Texas, USA. Jean Storlie M. Research Associate Research Associate. Institute for Behavioral Education King of Prussia, Pennsylvania, USA. Henry A. Jordan M. Director Director. Reprints and permissions. Practical Methods of Measuring Body Composition. In: Storlie, J. eds Evaluation and Treatment of Obesity. Sports Medicine and Health Science. Springer, Dordrecht. Publisher Name : Springer, Dordrecht. Print ISBN : Online ISBN : eBook Packages : Springer Book Archive. Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Policies and ethics. Skip to main content. Abstract Body composition is an important component of exercise prescription and health management programs. Keywords Body Composition Body Density Mass Testing Anthropometric Variable Measure Body Composition These keywords were added by machine and not by the authors. Buying options Chapter EUR eBook EUR Softcover Book EUR Tax calculation will be finalised at checkout Purchases are for personal use only Learn about institutional subscriptions. Preview Unable to display preview. References Behnke, A. Google Scholar Jackson, A. Article PubMed CAS Google Scholar Jackson, A. CAS Google Scholar Brozek, J. Article PubMed CAS Google Scholar Sloan, A. PubMed CAS Google Scholar Sloan, A. Google Scholar Young, C. CAS Google Scholar Young, C. Article PubMed CAS Google Scholar Young, C. CAS Google Scholar Baumgartner, T. Google Scholar Pollock, M. PubMed CAS Google Scholar Pollock, M. PubMed CAS Google Scholar Durnin, J. Google Scholar Siri, W. |
| Body composition | BIA, L3-targeted CT, and DEXA represent the techniques of choice to evaluate body composition in clinical practice fig. In the setting of cost-effective and pragmatic use, these three techniques should be alternatively chosen. In cancer, undernourished, and nutritionally at-risk patients, an abdominal CT should be completed by the analysis of L3-targeted images for the evaluation of body composition. In other situations, BIA appears to be the simplest most reproducible and less expensive method, while DEXA, if feasible, remains the reference method for clinical practice. By allowing earlier management of undernutrition, body composition evaluation can contribute to reducing malnutrition-induced morbidity and mortality, improving the quality of life and, as a consequence, increasing the medico-economic benefits fig. The latter needs to be demonstrated. Moreover, based on a more scientific approach, i. allowing for printing reports, objective initial assessment and follow-up of nutritional status, and the adjustment of drug doses, body composition evaluation would contribute to a better recognition of the activities related to nutritional evaluation and care by the medical community, health care facilities, and health authorities fig. Screening of undernutrition is insufficient to allow for optimal nutrition care. This is in part due to the lack of sensitivity of BMI and weight loss for detecting FFM loss in patients with chronic diseases. Methods of body composition evaluation allow a quantitative measurement of FFM changes during the course of disease and could be used to detect FFM loss in the setting of an objective, systematic, and early undernutrition screening. FFM loss is closely related to impaired clinical outcomes, survival, and quality of life, as well as increased therapy toxicity in cancer patients. Thus, body composition evaluation should be integrated into clinical practice for the initial assessment, sequential follow-up of nutritional status, and the tailoring of nutritional and disease-specific therapies. Body composition evaluation could contribute to strengthening the role and credibility of nutrition in the global medical management, reducing the negative impact of malnutrition on the clinical outcome and quality of life, thereby increasing the overall medico-economic benefits. Thibault and C. Pichard are supported by research grants from the public foundation Nutrition Plus. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Annals of Nutrition and Metabolism. Advanced Search. Skip Nav Destination Close navigation menu Article navigation. Volume 60, Issue 1. Rationale for a New Strategy for the Screening of Undernutrition. Body Composition Evaluation for the Assessment of Nutritional Status. Body Composition Evaluation for the Calculation of Energy Needs. Body Composition Evaluation for the Follow-Up and Tailoring of Nutritional Support. Body Composition Evaluation for Tailoring Medical Treatments. Towards the Implementation of Body Composition Evaluation in Clinical Practice. Disclosure Statement. Article Navigation. Review Articles December 16 The Evaluation of Body Composition: A Useful Tool for Clinical Practice Subject Area: Endocrinology , Further Areas , Nutrition and Dietetics , Public Health. Ronan Thibault ; Ronan Thibault. a Centre de Recherche en Nutrition Humaine Auvergne, UMR Nutrition Humaine, INRA, Clermont Université, Service de Nutrition Clinique, CHU de Clermont-Ferrand, Clermont-Ferrand, France;. This Site. Google Scholar. Claude Pichard Claude Pichard. b Nutrition Unit, Geneva University Hospital, Geneva, Switzerland. Ann Nutr Metab 60 1 : 6— Article history Received:. Cite Icon Cite. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. View large Download slide. Table 1 Main reasons for the lack of nutritional screening at hospitals. View large. View Large. Table 2 Mean values of body composition compartments adapted from Pichard and Kyle [ 19 and Wang et al. Ronan Thibault and Claude Pichard declare no conflict of interest. Pirlich M, Schutz T, Norman K, Gastell S, Lübke HJ, Bischoff SC, Bolder U, Frieling T, Güldenzoph H, Hahn K, Jauch KW, Schindler K, Stein J, Volkert D, Weimann A, Werner H, Wolf C, Zürcher G, Bauer P, Lochs H: The German hospital malnutrition study. Clin Nutr ;— Amaral TF, Matos LC, Tavares MM, Subtil A, Martins R, Nazaré M, Sousa Pereira N: The economic impact of disease-related malnutrition at hospital admission. Pichard C, Kyle UG, Morabia A, Perrier A, Vermeulen B, Unger P: Nutritional assessment: lean body mass depletion at hospital admission is associated with increased length of stay. Am J Clin Nutr ;— Capuano G, Gentile PC, Bianciardi F, Tosti M, Palladino A, Di Palma M: Prevalence and influence of malnutrition on quality of life and performance status in patients with locally advanced head and neck cancer before treatment. Support Care Cancer ;— Prado CM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, Martin L, Baracos VE: Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol ;— Tan BHL, Birdsell LA, Martin L, Baracos VE, Fearon KC: Sarcopenia in an overweight or obese patient is an adverse prognostic factor in pancreatic cancer. Clin Cancer Res ;— Baracos VE, Reiman T, Mourtzakis M, Gioulbasanis I, Antoun S: Body composition in patients with non-small cell lung cancer: a contemporary view of cancer cachexia with the use of computed tomography image analysis. Am J Clin Nutr ;91 suppl : S—S. Antoun S, Baracos VE, Birdsell L, Escudier B, Sawyer MB: Low body mass index and sarcopenia associated with dose-limiting toxicity of sorafenib in patients with renal cell carcinoma. Ann Oncol ;— Prado CM, Baracos VE, McCargar LJ, Mourtzakis M, Mulder KE, Reiman T, Butts CA, Scarfe AG, Sawyer MB: Body composition as an independent determinant of 5-fluorouracil-based chemotherapy toxicity. Prado CM, Baracos VE, McCargar LJ, Reiman T, Mourtzakis M, Tonkin K, Mackey JR, Koski S, Pituskin E, Sawyer MB: Sarcopenia as a determinant of chemotherapy toxicity and time to tumor progression in metastatic breast cancer patients receiving capecitabine treatment. Hofhuis JG, Spronk PE, van Stel HF, Schrijvers GJ, Rommes JH, Bakker J: The impact of critical illness on perceived health-related quality of life during ICU treatment, hospital stay, and after hospital discharge: a long-term follow-up study. Chest ;— Guest JF, Panca M, Baeyens JP, de Man F, Ljungqvist O, Pichard C, Wait S, Wilson L: Health economic impact of managing patients following a community-based diagnosis of malnutrition in the UK. Kyle UG, Morabia A, Slosman DO, Mensi N, Unger P, Pichard C: Contribution of body composition to nutritional assessment at hospital admission in patients: a controlled population study. Br J Nutr ;— Kondrup J, Allison SP, Elia M; Vellas B, Plauth M: Educational and Clinical Practice Committee, European Society of Parenteral and Enteral Nutrition ESPEN : ESPEN guidelines for nutrition screening Haute Autorité de Santé: IPAQSS: informations. World Health Organization: Obesity and overweight: fact sheet No. Thibault R, Chikhi M, Clerc A, Darmon P, Chopard P, Picard-Kossovsky M, Genton L, Pichard C: Assessment of food intake in hospitalised patients: a 10 year-comparative study of a prospective hospital survey. Stenholm S, Harris TB, Rantanen T, Visser M, Kritchevsky SB, Ferrucci L: Sarcopenic obesity: definition, cause and consequences. Curr Opin Clin Nutr Metab Care ;— Pichard C, Kyle UG: Body composition measurements during wasting diseases. Wang ZM, Pierson RN Jr, Heymsfield SB: The five-level model: a new approach to organizing body-composition research. Schols AM, Broekhuizen R, Weling-Scheepers CA, Wouters EF: Body composition and mortality in chronic obstructive pulmonary disease. Slinde F, Gronberg A, Engstrom CP, Rossander-Hulthen L, Larsson S: Body composition by bioelectrical impedance predicts mortality in chronic obstructive pulmonary disease patients. Respir Med ;— Vestbo J, Prescott E, Almdal T, Dahl M, Nordestgaard BG, Andersen T, Sorensen TI, Lange P: Body mass, fat-free body mass, and prognosis in patients with chronic obstructive pulmonary disease from a random population sample: findings from the Copenhagen City Heart Study. Am J Respir Crit Care Med ;— Segall L, Mardare NG, Ungureanu S, Busuioc M, Nistor I, Enache R, Marian S, Covic A: Nutritional status evaluation and survival in haemodialysis patients in one centre from Romania. Nephrol Dial Transplant ;— Beddhu S, Pappas LM, Ramkumar N, Samore M: Effects of body size and body composition on survival in hemodialysis patients. J Am Soc Nephrol ;— Fürstenberg A, Davenport A: Assessment of body composition in peritoneal dialysis patients using bioelectrical impedance and dual-energy X-ray absorptiometry. Am J Nephrol ;— Futter JE, Cleland JG, Clark AL: Body mass indices and outcome in patients with chronic heart failure. Eur J Heart Fail ;— Marin B, Desport JC, Kajeu P, Jesus P, Nicolaud B, Nicol M, Preux PM, Couratier P: Alteration of nutritional status at diagnosis is a prognostic factor for survival of amyotrophic lateral sclerosis patients. J Neurol Neurosurg Psychiatry ;— Janiszewski PM, Oeffinger KC, Church TS, Dunn AL, Eshelman DA, Victor RG, Brooks S, Turoff AJ, Sinclair E, Murray JC, Bashore L, Ross R: Abdominal obesity, liver fat, and muscle composition in survivors of childhood acute lymphoblastic leukemia. J Clin Endocrinol Metab ;— Wagner D, Adunka C, Kniepeiss D, Jakoby E, Schaffellner S, Kandlbauer M, Fahrleitner-Pammer A, Roller RE, Kornprat P, Müller H, Iberer F, Tscheliessnigg KH: Serum albumin, subjective global assessment, body mass index and the bioimpedance analysis in the assessment of malnutrition in patients up to 15 years after liver transplantation. Clin Transplant ;E—E Kimyagarov S, Klid R, Levenkrohn S, Fleissig Y, Kopel B, Arad M, Adunsky A: Body mass index BMI , body composition and mortality of nursing home elderly residents. Arch Gerontol Geriatr ;— J Nutr Health Aging ;— Schols AM, Wouters EF, Soeters PB, Westerterp KR: Body composition by bioelectrical-impedance analysis compared with deuterium dilution and skinfold anthropometry in patients with chronic obstructive pulmonary disease. Thibault R, Le Gallic E, Picard-Kossovsky M, Darmaun D, Chambellan A: Assessment of nutritional status and body composition in patients with COPD: comparison of several methods in French. Rev Mal Respir ;— Kyle UG, Janssens JP, Rochat T, Raguso CA, Pichard C: Body composition in patients with chronic hypercapnic respiratory failure. Rieken R, van Goudoever JB, Schierbeek H, Willemsen SP, Calis EA, Tibboel D, Evenhuis HM, Penning C: Measuring body composition and energy expenditure in children with severe neurologic impairment and intellectual disability. Kidney Int Suppl ;S37—S Frisancho AR: New norms of upper limb fat and muscle areas for assessment of nutritional status. Caregaro L, Alberino F, Amodio P, Merkel C, Bolognesi M, Angeli P, Gatta A: Malnutrition in alcoholic and virus-related cirrhosis. Am J Clin Nutr l;— Alberino F, Gatta A, Amodio P, Merkel C, Di Pascoli L, Boffo G, Caregaro L: Nutrition and survival in patients with liver cirrhosis. Nutrition ;— Liu E, Spiegelman D, Semu H, Hawkins C, Chalamilla G, Aveika A, Nyamsangia S, Mehta S, Mtasiwa D, Fawzi W: Nutritional status and mortality among HIV-infected patients receiving antiretroviral therapy in Tanzania. J Infect Dis ;— Soler-Cataluna JJ, Sanchez-Sanchez L, Martinez-Garcia MA, Sanchez PR, Salcedo E, Navarro M: Mid-arm muscle area is a better predictor of mortality than body mass index in COPD. Marquis K, Debigaré R, Lacasse Y, LeBlanc P, Jobin J, Carrier G, Maltais F: Midthigh muscle cross-sectional area is a better predictor of mortality than body mass index in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med ;15;— Kyle UG, Pirlich M, Lochs H, Schuetz T, Pichard C: Increased length of hospital stay in underweight and overweight patients at hospital admission: a controlled population study. Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gómez JM, Heitmann BL, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, Schols AM, Pichard C, Composition of the ESPEN Working Group. Bioelectrical impedance analysis. Review of principles and methods. Santarpia L, Marra M, Montagnese C, Alfonsi L, Pasanisi F, Contaldo F: Prognostic significance of bioelectrical impedance phase angle in advanced cancer: preliminary observations. Gupta D, Lammersfeld CA, Vashi PG, King J, Dahlk SL, Grutsch JF, Lis CG: Bioelectrical impedance phase angle in clinical practice: implications for prognosis in stage IIIB and IV non-small cell lung cancer. BMC Cancer ; Gupta D, Lis CG, Dahlk SL, Vashi PG, Grutsch JF, Lammersfeld CA: Bioelectrical impedance phase angle as a prognostic indicator in advanced pancreatic cancer. Gupta D, Lammersfeld CA, Burrows JL, Dahlk SL, Vashi PG, Grutsch JF, Hoffman S, Lis CG: Bioelectrical impedance phase angle in clinical practice: implications for prognosis in advanced colorectal cancer. Paiva SI, Borges LR, Halpern-Silveira D, Assunção MC, Barros AJ, Gonzalez MC: Standardized phase angle from bioelectrical impedance analysis as prognostic factor for survival in patients with cancer. Schwenk A, Beisenherz A, Römer K, Kremer G, Salzberger B, Elia M: Phase angle from bioelectrical impedance analysis remains an independent predictive marker in HIV-infected patients in the era of highly active antiretroviral treatment. Desport JC, Marin B, Funalot B, Preux PM, Couratier P: Phase angle is a prognostic factor for survival in amyotrophic lateral sclerosis. Amyotroph Lateral Scler ;— Wirth R, Volkert D, Rösler A, Sieber CC, Bauer JM: Bioelectric impedance phase angle is associated with hospital mortality of geriatric patients. Mushnick R, Fein PA, Mittman N, Goel N, Chattopadhyay J, Avram MM: Relationship of bioelectrical impedance parameters to nutrition and survival in peritoneal dialysis patients. Kidney Int Suppl ;S53—S Selberg O, Selberg D: Norms and correlates of bioimpedance phase angle in healthy human subjects, hospitalized patients, and patients with liver cirrhosis. Eur J Appl Physiol ;— Shah S, Whalen C, Kotler DP, Mayanja H, Namale A, Melikian G, Mugerwa R, Semba RD: Severity of human immunodeficiency virus infection is associated with decreased phase angle, fat mass and body cell mass in adults with pulmonary tuberculosis infection in Uganda. J Nutr ;— Barbosa-Silva MC, Barros AJ: Bioelectric impedance and individual characteristics as prognostic factors for post-operative complications. Durnin JV, Womersley J: Body fat assessed from total body density and its estimation from skinfold thickness: measurements on men and women aged from 16 to 72 years. Hill GL: Body composition research: implications for the practice of clinical nutrition. JPEN J Parenter Enter Nutr ;— Pierson RN Jr, Wang J, Thornton JC, Van Itallie TB, Colt EW: Body potassium by four-pi 40K counting: an anthropometric correction. Am J Physiol ;F—F Sohlström A, Forsum E: Changes in total body fat during the human reproductive cycle as assessed by magnetic resonance imaging, body water dilution, and skinfold thickness: a comparison of methods. Leonard CM, Roza MA, Barr RD, Webber CE: Reproducibility of DXA measurements of bone mineral density and body composition in children. Pediatr Radiol ;— Genton L, Karsegard VL, Zawadynski S, Kyle UG, Pichard C, Golay A, Hans DB: Comparison of body weight and composition measured by two different dual energy X-ray absorptiometry devices and three acquisition modes in obese women. Jaffrin MY: Body composition determination by bioimpedance: an update. Kyle UG, Pichard C, Rochat T, Slosman DO, Fitting JW, Thiebaud D: New bioelectrical impedance formula for patients with respiratory insufficiency: comparison to dual-energy X-ray absorptiometry. Eur Respir J ;— Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Manuel Gómez J, Lilienthal Heitmann B, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, Schols AMWJ, Pichard C, ESPEN: Bioelectrical impedance analysis. Utilization in clinical practice. Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE: A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab ;— Bolton CE, Ionescu AA, Shiels KM, Pettit RJ, Edwards PH, Stone MD, Nixon LS, Evans WD, Griffiths TL, Shale DJ: Associated loss of fat-free mass and bone mineral density in chronic obstructive pulmonary disease. Kyle UG, Genton L, Karsegard L, Slosman DO, Pichard C: Single prediction equation for bioelectrical impedance analysis in adults aged 20—94 years. Kyle UG, Genton L, Slosman DO, Pichard C: Fat-free and fat mass percentiles in 5, healthy subjects aged 15 to 98 years. Nutrition ;17 7—8 — Kotler DP, Burastero S, Wang J, Pierson RN Jr: Prediction of body cell mass, fat-free mass, and total body water with bioelectrical impedance analysis: effects of race, sex, and disease. Am J Clin Nutr ;S—S. Kyle UG, Genton L, Mentha G, Nicod L, Slosman DO, Pichard C: Reliable bioelectrical impedance analysis estimate of fat-free mass in liver, lung, and heart transplant patients. JPEN J Parenter Enteral Nutr ;— Mattar L, Godart N, Melchior JC, Falissard B, Kolta S, Ringuenet D, Vindreau C, Nordon C, Blanchet C, Pichard C: Underweight patients with anorexia nervosa: comparison of bioelectrical impedance analysis using five equations to dual X-ray absorptiometry. Clin Nutr , E-pub ahead of print. Genton L, Karsegard VL, Kyle UG, Hans DB, Michel JP, Pichard C: Comparison of four bioelectrical impedance analysis formulas in healthy elderly subjects. Gerontology ;— Robert S, Zarowitz BJ, Hyzy R, Eichenhorn M, Peterson EL, Popovich J Jr: Bioelectrical impedance assessment of nutritional status in critically ill patients. Pichard C, Kyle UG, Slosman DO, Penalosa B: Energy expenditure in anorexia nervosa: can fat-free mass as measured by bioelectrical impedance predict energy expenditure in hospitalized patients? Kreymann KG, Berger MM, Deutz NE, Hiesmayr M, Jolliet P, Kazandjiev G, Nitenberg G, van den Berghe G, Wernerman J, DGEM German Society for Nutritional Medicine , Ebner C, Hartl W, Heymann C, Spies C, ESPEN: ESPEN guidelines on enteral nutrition: intensive care. Singer P, Berger MM, van den Berghe G, Biolo G, Calder P, Forbes A, Griffiths R, Kreyman G, Leverve X, Pichard C, ESPEN: ESPEN guidelines on parenteral nutrition: intensive care. Magnuson B, Peppard A, Auer Flomenhoft D: Hypocaloric considerations in patients with potentially hypometabolic disease states. Nutr Clin Pract ;— Rigaud D, Boulier A, Tallonneau I, Brindisi MC, Rozen R: Body fluid retention and body weight change in anorexia nervosa patients during refeeding. Kyle UG, Chalandon Y, Miralbell R, Karsegard VL, Hans D, Trombetti A, Rizzoli R, Helg C, Pichard C: Longitudinal follow-up of body composition in hematopoietic stem cell transplant patients. Bone Marrow Transplant ;— Pison CM, Cano NJ, Cherion C, Caron F, Court-Fortune I, Antonini M, Gonzalez-Bermejo J, Meziane L, Molano LC, Janssens JP, Costes F, Wuyam B, Similowski T, Melloni B, Hayot M, Augustin J, Tardif C, Lejeune H, Roth H, Pichard C, the IRAD Investigators: Multimodal nutritional rehabilitation improves clinical outcomes of malnourished patients with chronic respiratory failure: a controlled randomised trial. Thorax ;— Pichard C, Kyle U, Chevrolet JC, Jolliet P, Slosman D, Mensi N, Temler E, Ricou B: Lack of effects of recombinant growth hormone on muscle function in patients requiring prolonged mechanical ventilation: a prospective, randomized, controlled study. Crit Care Med ;— Pichard C, Kyle UG, Jolliet P, Slosman DO, Rochat T, Nicod L, Romand J, Mensi N, Chevrolet JC: Treatment of cachexia with recombinant growth hormone in a patient before lung transplantation: a case report. Leslie WD, Miller N, Rogala L, Bernstein CN: Body mass and composition affect bone density in recently diagnosed inflammatory bowel disease: the Manitoba IBD Cohort Study. Inflamm Bowel Dis ;— van der Meij BS, Langius JA, Smit EF, Spreeuwenberg MD, von Blomberg BM, Heijboer AC, Paul MA, van Leeuwen PA: Oral nutritional supplements containing n-3 polyunsaturated fatty acids affect the nutritional status of patients with stage III non-small cell lung cancer during multimodality treatment. Ryan AM, Reynolds JV, Healy L, Byrne M, Moore J, Brannelly N, McHugh A, McCormack D, Flood P: Enteral nutrition enriched with eicosapentaenoic acid EPA preserves lean body mass following esophageal cancer surgery: results of a double-blinded randomized controlled trial. Ann Surg ;— Ndekha MJ, Oosterhout JJ, Zijlstra EE, Manary M, Saloojee H, Manary MJ: Supplementary feeding with either ready-to-use fortified spread or corn-soy blend in wasted adults starting antiretroviral therapy in Malawi: randomised, investigator blinded, controlled trial. BMJ ;b—b Ha L, Hauge T, Iversen PO: Body composition in older acute stroke patients after treatment with individualized, nutritional supplementation while in hospital. BMC Geriatrics ; Body composition of participants 70 women and men, age: Multiple regression analysis was used to develop equations predicting AT and ATFM from these three single slices. This simplified method allows a fully accurate assessment of the body composition of people with obesity in less than 20 min 10 min for images acquisition and analysis, respectively , useful for a follow-up. Obesity is a major public health issue 1. The consequences are numerous and include cardiovascular diseases, metabolic syndrome, non-alcoholic fatty liver disease and obstructive sleep apnea 2 , 3 , 4 , 5. These adverse outcomes increasingly affect adults and children 1 , 6 , 7. Magnetic resonance imaging MRI is the gold standard 16 , 17 , 18 , 19 , 20 , 21 to quantify skeletal muscle and adipose tissue, and to assess its distribution. Owing to the relatively high cost of MRI 22 and the elevated image-acquisition time attributed to multi-slice imaging 16 , a single slice at the abdomen is often used in various clinical settings 14 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , However, this measure is not sensitive to interindividual morphological differences, in particular fat distribution e. android or gynoid obesity Moreover, fat evaluation at the thoracic level T6-T7 34 may represent a good assessment of thoracic obesity independently of sex Although visceral fat is correlated with obesity-related diseases 9 , 11 , 12 , 15 , 36 , it is important to analyze whole-body composition to thoroughly assess the effects of different interventions such as exercise and diet in clinical settings. A very interesting study showed that a single slice at L3 was the best compromise to assess total tissue volumes of whole-body skeletal muscle, VAT, and SAT However, the authors reported a lack of sensitivity to track changes of body composition probably because of lack of specificity of this slice. A mid-thigh slice has been shown to reflect whole-body muscle mass in both obese 38 and normal-weight individuals 27 , 38 , Moreover, Schweitzer et al. L3, and that during a follow-up with weight-loss changes, unsurprisingly, the area at L3 reflected changes in total VAT and SAT. These results lead the authors to conclude that areas at mid-thigh showed the best evidence to assess changes in total skeletal volume. Taken together these results and ours suggest that the best way to quickly and accurately estimate and follow adipose tissue and adipose tissues free mass was to incorporate 3 single slices in a model. To achieve this goal, we tested the concordance and agreement between the predictive and the measured body composition in a subgroup of people of both sexes with overweight and obesity. We also aimed to assess the sensitivity of equations to detect changes in body composition induced by an aerobic exercise training program. We hypothesized that body composition would be accurately assessed and followed up over time in people with overweight and obesity using predictive equations. Thirty-eight participants had a BMI lower than 25 kg. We used data from a completed clinical trial NCT testing the cardiometabolic effects of different exercise training modalities i. Body composition was assessed before T0 and after the 2-month T2 training period. The study was approved by the local ethics committee Comité de Protection des Personnes Sud-Est V and performed according to the Declaration of Helsinki. Participants were informed of the procedure and risks involved and gave their written consent prior to all assessments. MRI is a reference method for assessing body composition including AT, ATFM and its regional distribution, and particularly visceral adipose tissue 16 , In order to determine full body composition called measured body composition , the reference method includes 41 slices with a thickness of 10 mm spaced by 40 mm MRI data were acquired in 30 min for each participant on a General Electric Signa Advantage 1. For the specific purpose of the present study prediction of body composition , three single slices thickness of 10 mm were acquired in 10 min at 3 different localizations: T6-T7, L4-L5 and mid-thigh. Mid-thigh level for the single slice acquisition was determined by computing half of the overall femoral length. In our medical department, we used our own equation unpublished results to measure the half-femoral length. Indeed, statistical analysis of different populations shows that the stature can be derived from the femoral length We compared the formula used in our medical department to those available in the literature The average difference of half-femoral length between our method and the one described in Trotter was only of 0. Each slice was analyzed using Matlab-based software Matlab ® , Mathworks, Inc. developed by the radiology department of University Hospital of Grenoble Alps. The brightness level of tissue distinguished AT and ATFM, using the graphical interface of Matlab ®. More specifically, we measured adipose tissue and calculated adipose tissue free mass by subtracting adipose tissue area to slice area. Moreover, determination of tissue area on a given MR image is performed by subjecting the data to various segmentation techniques. In our laboratory we have developed a computer software specifically designed for MR image analysis similar to that developed by Ross et al. The program features an interactive slice editor routine that allows for the verification of the segmentation result. This feature helps to assure that the area cm 2 values for the tissues of interest are accurately and reliably measured. Each slice was visually controlled to avoid an error in tissue type assignment, after histogram analysis to define a threshold for fat tissue segmentation. As our goal was to measure two types of tissues: adipose and adipose tissue free mass, we used a simplified method derived from the one developed by Ross et al. After threshold definition, the segmented image was compared to the MR image to correct wrong tissue type assignment when necessary. For instance, small isolated white dots occurring for instance when the slice concerned only a very small amount of isolated adipose tissue so-called partial volume effect were not considered in the AT amount. On the other side, weak MR signals occurring sometimes in the subcutaneous fat tissues were manually added to the AT. As initial double blinded initial tests did not result in significant differences, we considered that the AT amount measurement process was reliable. To calculate the adipose tissue and lean tissue volumes in each slice, the program multiplies the number of pixels by the pixel surface cm 2 and the thickness 10 mm of the slice. Whole-body adipose tissue and lean tissue volumes were calculated using the truncated pyramid method At last, the volume in liters of adipose tissue and lean tissue was converted to mass kg by multiplying the volumes of the assumed constant density of 0. The inter-observer variability was respectively 2. We tested the sensitivity of the prediction model on 79 participants with overweight or obesity following two isocaloric aerobic exercise training programs known to significantly induce adipose tissue loss For this reason, we did not distinguish the effects of the two modalities in the statistical analysis. Specifically, participants were installed on an electronically braked cycle ergometer Corival, Lode B. Multiple linear regression analysis was performed to assess the relation between the measured AT or ATFM by the 41 slices and those predicted by the three single slices. The R 2 was adjusted for the number of predictors. We used an automated variable selection procedure for forward, backward, and stepwise variable selection using the AIC Akaike information criterion estimator which evaluates the quality of each model, relative to each of the other models Comparison between the predicted and measured AT and ATFM was performed using t -tests. Levels closer to 1 indicate better agreement between methods. Sensitivity of the prediction models to an exercise training program was also studied. Data were statistically analyzed using the nonparametric test Wilcoxon to compare the variations between the MRI reference method and the predictive method before T0 and after 2-months T2 of exercise training program. The statistical software R version 3. The 3 single MRI slices at T6-T7, L4-L5 and mid-thigh , sex, age, weight and height of participants were included in linear regression models as independent variables, with total AT as the dependent variable Table 2. Without height, predicted AT was more strongly correlated with measured AT with an adjusted R 2 of There was no significant difference between predicted and measured AT measured: Bland—Altman plots illustrate the difference between predicted and measured AT in people with overweight total: 0. Bland—Altman plot agreement of adipose tissue AT A and adipose tissue free mass ATFM B in overweight people. Bland—Altman plot agreement of adipose tissue AT A and adipose tissue free mass ATFM B in people with obesity. The same analysis was applied to the dependent variable total ATFM. Multiple regression equations for estimation of total ATFM were developed Table 2. There was no significant difference between predicted and measured ATFM measured: The measured and predicted AT after 2-months T2 of exercise training did not significantly differ compared to baseline T0 T2: measured: T0: measured: The same result was observed for ATFM variation T2: measured: Our results showed that the best fit models that we developed had a high adjusted R 2 AT: The SEE of our predictive equation compared quite well with that used by Schweitzer et al. Indeed, in the present study we built our equation in a population with obesity subjects with overweight or obesity out of In an attempt to predict total subcutaneous adipose tissue with a single slice at L3, Schweitzer et al. Regarding ATFM, they reported R 2 between 0. Overall, despite greater SEE for ATFM, our equations seem better than those reported in literature and our model represents a breakthrough in the rapid estimation of body composition by MRI in overweight and obesity. This is a progress compared to other simplified approaches of body composition such as anthropometrics. Indeed, Lee et al. In addition, when the predictive model of Lee et al. According to the authors, this could be due to the fact that inter- and intra-muscular adipose tissue could not be distinguished by anthropometric measurements including skinfold thickness Hence, the prediction of body composition from MRI single slices seems more appropriate and accurate. Therefore, it seems that the best-fit equations can be used in a range of different profiles to quickly and accurately analyze body composition. A larger sample size in this subgroup might have provided higher concordance between predicted and measured methods. There are several possibilities to explain the good concordance and agreement in these subgroups, including, the representativeness of the different types of obesity and the choice of three area slices. The included participants also varied in age range: 20—81, Despite the heterogeneity of the studied population, the best-fit models that we developed gave a good prediction of AT and ATFM in both men and women and in varying BMI between 25 kg. Secondly, over the last few years a single abdominal slice has been proposed to predict total fat and lean masses 27 and to quickly assess subcutaneous adipose tissue and visceral adipose tissue 23 , 24 , 25 , 26 , 27 , 31 , which provides complementary information regarding cardiometabolic risk. One of the major drawbacks of this method was that a single slice cannot take into account the interindividual morphological differences e. Accordingly, three single slices at T6-T7, L4-L5 and mid-thigh seems to be a good compromise between the time to analyze 20 min and the accuracy of body composition prediction. Recently, other localizations have been proposed to assess subcutaneous adipose tissue and visceral adipose tissue particularly around L3 25 , 26 , 27 , 28 while L4-L5 was used in the present study. Maislin et al. This localization could decrease the standard error and improve the precision of our models. However, this remains to be tested. The mid-thigh has also been described as an optimal slice area to assess total ATFM Such a measurement would be for instance relevant to detect sarcopenic obesity. To the best of our knowledge, no study has investigated one common localization to assess AT and ATFM in the thoracic area. Hence, the single MRI slice at T6-T7 has been arbitrarily chosen hoping that it will the best site to determine, especially the mammary fat However, the localization of these three slices does not allow for the evaluation of fat in the gluteo-femoral region. This region is an area in which women with obesity often accumulate adipose tissue 21 , 33 , Thus, adding an MRI slice below the iliac crest could be relevant. Whatever the method measured or predictive , no significant modification of body composition was induced by 2 months of exercise training on ergocycle. A meta-analysis of Batacan et al. In the present study, we cannot definitely conclude on the potential sensitivity of our prediction models because we did not observe a modification of body composition. However, there was no significant difference between measured or predictive method after 2-months of intervention indicating at least that the 2 measurement methods are not discordant. Of note, estimating body composition with a unique slice at L3 level failed to track changes of body composition probably in persons losing weight because of lack of specificity of this slice The choice of a body composition method depends on the accuracy and precision needed. However, the acquisition time is also important to allow its use in a routine clinical setting as well as for research purposes. With the predictive method, the time required to collect 10 min and to analyze 10 min MRI images is well below the reference MRI method 20 min vs. The associated gain in time and the reduced cost of this evaluation are crucial in a clinical research setting. The choice of the methods also depends on the target population. For example, our model may not be generalizable to different patient populations who have specific body composition e. COPD or highly trained athletes. For that reason, other predictive models must be developed for each specific population. Of course, an interesting perspective, could be to use the adipose tissue free mass and adipose tissue of the different slices locations T6-T7, L4-L5 and at mid-thigh to better characterize the various profiles of obesity android, gynoid and the associated cardiovascular risk. However, such a perspective could not be envisaged at the present condition since we did not measure the biological markers of this cardiovascular risk. In conclusion, predictive equations with three MRI slices T6-T7, L4-L5 and mid-thigh were effective to quickly and accurately assess the body composition of people with overweight or obesity compared to the reference methods. The findings we herein report have thus the potential to contribute to a fast and reliable estimation of AT and ATFM in overweight or obesity in clinical routine. Di Cesare, M. et al. Trends in adult BMI in countries from to Lancet , — Google Scholar. Alam, I. Obesity metabolic syndrome and sleep apnoea: All pro-inflammatory states. Article Google Scholar. Faria, A. Impact of visceral fat on blood pressure and insulin sensitivity in hypertensive obese women. Article PubMed Google Scholar. Karlas, T. Gastrointestinal complications of obesity: Nonalcoholic fatty liver disease NAFLD and its sequelae. Best Pract Res Clin Endocrinol Metab. Article CAS PubMed Google Scholar. Schäfer, H. Body fat distribution, serum leptin, and cardiovascular risk factors in men with obstructive sleep apnea. Chest 3 , — Flegal, K. Prevalence and trends in obesity among US adults, — JAMA 3 , — INSERM Institut National de la Santé et de la Recherche Médicale , Obépi, enquête épidémiologique nationale sur le surpoids et l'obésité. Tzankoff, S. Effect of muscle mass decrease on age-related BMR changes. Kuk, J. Visceral fat is an independent predictor of all-cause mortality in men. Obesity 14 2 , — Measurement site and the association between visceral and abdominal subcutaneous adipose tissue with metabolic risk in women. Obesity 18 7 , — Machann, J. Standardized assessment of whole body adipose tissue topography by MRI. Imaging 21 , — Rissanen, J. Visceral adiposity androgens and plasma lipids in obese men. Metabolism 43 10 , — Ross, R. Influence of diet and exercise on skeletal muscle and visceral adipose tissue in men. Shen, W. A single MRI slice does not accurately predict visceral and subcutaneous adipose tissue changes during weight loss. Obesity 20 12 , — Von Eyben, F. Computed tomography scans of intra-abdominal fat, anthropometric measurements, and 3 nonobese metabolic risk factors. Magnetic resonance imaging provides new insights into the characterization of adipose and lean tissue distribution. Heymsfield, S. Human body composition: Advances in models and methods. Prado, C. Lean tissue imaging: A new era for nutritional assessment and intervention. Enteral 38 8 , — Quantification of adipose tissue by MRI: Relationship with anthropometric variables. Article MathSciNet CAS PubMed Google Scholar. Adipose tissue distribution measured by magnetic resonance imaging in obese women. Ayvaz, G. Methods for body composition analysis in adults. |
Body composition evaluation method -
More information is needed about the accuracy of these methods. Multi-compartment models are considered to be the most accurate method of body composition assessment 3 , These models split the body into three or more parts.
The most common assessments are called 3-compartment and 4-compartment models. These models require multiple tests to get estimates of body mass, body volume, body water and bone content For example, hydrostatic weighing or ADP can provide body volume, BIS or BIA can provide body water and DXA can measure bone content.
Information from each of these methods is combined to build a more complete picture of the body and obtain the most accurate body fat percentage 21 , However, they involve multiple tests and are not typically available to the general public.
Some methods, such as skinfold measurements, circumference calculations and portable BIA devices, are inexpensive and allow you to be measured in your own home as frequently as you like.
The devices can also be purchased online easily, such as on Amazon. Most of the methods with highest accuracies are not available to use in your own home. If you want a more accurate assessment and are willing to pay for it, you could pursue a method with good accuracy like hydrostatic weighing, ADP or DXA.
Ideally, you should do the test before you have anything to drink, especially for methods that rely on electrical signals like BIA, BIS and EIM.
Assessing yourself the same way each time will reduce error rates and make it easier to tell if you are making progress. However, you should always interpret your results from any method with caution. Even the best methods are not perfect and only give you an estimate of your true body fat.
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Several dietary and lifestyle changes can help you burn body fat. Here are 12 great methods to promote long-term fat loss. It is a myth that a pound of body fat contains exactly 3, calories.
This article explains the actual amount and what that means for weight loss. This article takes a look at the science behind targeted fat loss, and checks if you can slim down specific areas of your body. If losing weight is your goal, this article covers 18 foods that may help support a healthy and sustainable weight loss journey, according to science.
Making a few small changes to your morning routine can help you lose weight and keep it off. This article tells you how. Exercise burns calories, but many people claim it doesn't help you lose weight. This article explores whether exercise really helps with weight loss.
Male body types are often divided into three types, determined by factors like limb proportions, weight, height, and body fat distribution. You can easily estimate your basal metabolic rate using the Mifflin-St. Jeor equation — or by using our quick calculator.
Here's how. Many think the pear body shape is healthier than the apple body shape. This article explains the pear and apple body shapes, the research behind them…. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep?
Health Conditions Discover Plan Connect. Nutrition Evidence Based The 10 Best Ways to Measure Your Body Fat Percentage. By Grant Tinsley, Ph. Share on Pinterest.
Skinfold Calipers. Body Circumference Measurements. Dual-Energy X-ray Absorptiometry DXA. Hydrostatic Weighing. Air Displacement Plethysmography Bod Pod. Bioelectrical Impedance Analysis BIA.
Bioimpedance Spectroscopy BIS. Electrical Impedance Myography EIM. Multi-Compartment Models the Gold Standard. Which Method Is Best for You? How we reviewed this article: History.
May 18, Written By Grant Tinsley, Ph. Share this article. Read this next. By Rachael Ajmera, MS, RD. How Many Calories Are in a Pound of Body Fat? Is It Possible to Target Fat Loss to Specific Body Parts?
By Jillian Kubala, MS, RD. By Lisa Wartenberg, MFA, RD, LD. Does Exercise Help You Lose Weight? The Surprising Truth. What Are the Three Male Body Types? READ MORE. Of these methods, one that is both accurate and practical is skinfold measurement.
The measurements are taken with calipers, which gauge the skinfold thickness in millimeters of areas where fat typically accumulates i. Once the measurements are recorded, the numbers are inserted into an equation that calculates a body fat percentage and alternatively body lean mass.
Skinfold is a preferred method of body fat measurement for non-clinical settings because it is easy to administer with proven accuracy and is not obtrusive with regards to the patient. It also provides much more data than just the final composition measurement - it also yields the thickness of many sites, which can be used as bases of comparison with future results.
For example, an abdominal skinfold improvement from 35mm to 24mm would show a significant improvement in that site even if the overall body fat percentage may have only reduced minimally. BMI is often mistaken as measurable guide to body fat. However, BMI is simply a weight to height ratio.
It is a tool for indicating weight status in adults and general health in large populations. BMI correlates mildly with body fat but when used in conjunction with a body fat measurement gives a very accurate presentation of your current weight status.
With that being said, an elevated BMI above 30 significantly increases your risk of developing long-term and disabling conditions such as hypertension, diabetes mellitus, gallstones, stroke, osteoarthritis, and some forms of cancer.
For adults over 20 years old, BMI typically falls into one of the above categories see table above. UC Davis Health School of Medicine Betty Irene Moore School of Nursing News Careers Giving.
menu icon Menu. Sports Medicine. Enter search words search icon Search × Enter search words Body Composition UC Davis Sports Medicine UC Davis Health.
UC Davis Health Sports Medicine Learning Center Body Composition. Body composition. Fundamentals With respect to health and fitness, body composition is used to describe the percentages of fat, bone and muscle in human bodies.
DXA body composition analysis Dual X-ray Absorptiometry DXA is a quick and pain free scan that can tell you a lot about your body.
Composition analysis available. Example analysis from a DXA scan PDF Fat: function, metabolism and storage Although body fat endures a negative reputation, fats and lipids play critical roles in the overall functioning of the body, such as in digestion and energy metabolism.
With respect to health and fitness, body composition is used Body composition evaluation method describe the percentages Bofy fat, bone Copmosition muscle in human bodies. The body fat percentage is Sesame seed benefits most interest because composjtion can be very helpful in assessing health. Because muscular tissue is denser that fat tissue, assessing ones body fat is necessary to determine the overall composition of the body, particularly when making health recommendations. Two people at the same height and same body weight may have different health issues because they have a different body composition. Dual X-ray Absorptiometry DXA is a quick and pain free scan that can tell you a lot about your body.Body composition evaluation method -
Wagner D, Adunka C, Kniepeiss D, Jakoby E, Schaffellner S, Kandlbauer M, Fahrleitner-Pammer A, Roller RE, Kornprat P, Müller H, Iberer F, Tscheliessnigg KH: Serum albumin, subjective global assessment, body mass index and the bioimpedance analysis in the assessment of malnutrition in patients up to 15 years after liver transplantation.
Clin Transplant ;E—E Kimyagarov S, Klid R, Levenkrohn S, Fleissig Y, Kopel B, Arad M, Adunsky A: Body mass index BMI , body composition and mortality of nursing home elderly residents. Arch Gerontol Geriatr ;— J Nutr Health Aging ;— Schols AM, Wouters EF, Soeters PB, Westerterp KR: Body composition by bioelectrical-impedance analysis compared with deuterium dilution and skinfold anthropometry in patients with chronic obstructive pulmonary disease.
Thibault R, Le Gallic E, Picard-Kossovsky M, Darmaun D, Chambellan A: Assessment of nutritional status and body composition in patients with COPD: comparison of several methods in French. Rev Mal Respir ;— Kyle UG, Janssens JP, Rochat T, Raguso CA, Pichard C: Body composition in patients with chronic hypercapnic respiratory failure.
Rieken R, van Goudoever JB, Schierbeek H, Willemsen SP, Calis EA, Tibboel D, Evenhuis HM, Penning C: Measuring body composition and energy expenditure in children with severe neurologic impairment and intellectual disability.
Kidney Int Suppl ;S37—S Frisancho AR: New norms of upper limb fat and muscle areas for assessment of nutritional status. Caregaro L, Alberino F, Amodio P, Merkel C, Bolognesi M, Angeli P, Gatta A: Malnutrition in alcoholic and virus-related cirrhosis. Am J Clin Nutr l;— Alberino F, Gatta A, Amodio P, Merkel C, Di Pascoli L, Boffo G, Caregaro L: Nutrition and survival in patients with liver cirrhosis.
Nutrition ;— Liu E, Spiegelman D, Semu H, Hawkins C, Chalamilla G, Aveika A, Nyamsangia S, Mehta S, Mtasiwa D, Fawzi W: Nutritional status and mortality among HIV-infected patients receiving antiretroviral therapy in Tanzania.
J Infect Dis ;— Soler-Cataluna JJ, Sanchez-Sanchez L, Martinez-Garcia MA, Sanchez PR, Salcedo E, Navarro M: Mid-arm muscle area is a better predictor of mortality than body mass index in COPD.
Marquis K, Debigaré R, Lacasse Y, LeBlanc P, Jobin J, Carrier G, Maltais F: Midthigh muscle cross-sectional area is a better predictor of mortality than body mass index in patients with chronic obstructive pulmonary disease.
Am J Respir Crit Care Med ;15;— Kyle UG, Pirlich M, Lochs H, Schuetz T, Pichard C: Increased length of hospital stay in underweight and overweight patients at hospital admission: a controlled population study.
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gómez JM, Heitmann BL, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, Schols AM, Pichard C, Composition of the ESPEN Working Group.
Bioelectrical impedance analysis. Review of principles and methods. Santarpia L, Marra M, Montagnese C, Alfonsi L, Pasanisi F, Contaldo F: Prognostic significance of bioelectrical impedance phase angle in advanced cancer: preliminary observations.
Gupta D, Lammersfeld CA, Vashi PG, King J, Dahlk SL, Grutsch JF, Lis CG: Bioelectrical impedance phase angle in clinical practice: implications for prognosis in stage IIIB and IV non-small cell lung cancer.
BMC Cancer ; Gupta D, Lis CG, Dahlk SL, Vashi PG, Grutsch JF, Lammersfeld CA: Bioelectrical impedance phase angle as a prognostic indicator in advanced pancreatic cancer. Gupta D, Lammersfeld CA, Burrows JL, Dahlk SL, Vashi PG, Grutsch JF, Hoffman S, Lis CG: Bioelectrical impedance phase angle in clinical practice: implications for prognosis in advanced colorectal cancer.
Paiva SI, Borges LR, Halpern-Silveira D, Assunção MC, Barros AJ, Gonzalez MC: Standardized phase angle from bioelectrical impedance analysis as prognostic factor for survival in patients with cancer.
Schwenk A, Beisenherz A, Römer K, Kremer G, Salzberger B, Elia M: Phase angle from bioelectrical impedance analysis remains an independent predictive marker in HIV-infected patients in the era of highly active antiretroviral treatment. Desport JC, Marin B, Funalot B, Preux PM, Couratier P: Phase angle is a prognostic factor for survival in amyotrophic lateral sclerosis.
Amyotroph Lateral Scler ;— Wirth R, Volkert D, Rösler A, Sieber CC, Bauer JM: Bioelectric impedance phase angle is associated with hospital mortality of geriatric patients.
Mushnick R, Fein PA, Mittman N, Goel N, Chattopadhyay J, Avram MM: Relationship of bioelectrical impedance parameters to nutrition and survival in peritoneal dialysis patients.
Kidney Int Suppl ;S53—S Selberg O, Selberg D: Norms and correlates of bioimpedance phase angle in healthy human subjects, hospitalized patients, and patients with liver cirrhosis.
Eur J Appl Physiol ;— Shah S, Whalen C, Kotler DP, Mayanja H, Namale A, Melikian G, Mugerwa R, Semba RD: Severity of human immunodeficiency virus infection is associated with decreased phase angle, fat mass and body cell mass in adults with pulmonary tuberculosis infection in Uganda.
J Nutr ;— Barbosa-Silva MC, Barros AJ: Bioelectric impedance and individual characteristics as prognostic factors for post-operative complications. Durnin JV, Womersley J: Body fat assessed from total body density and its estimation from skinfold thickness: measurements on men and women aged from 16 to 72 years.
Hill GL: Body composition research: implications for the practice of clinical nutrition. JPEN J Parenter Enter Nutr ;— Pierson RN Jr, Wang J, Thornton JC, Van Itallie TB, Colt EW: Body potassium by four-pi 40K counting: an anthropometric correction.
Am J Physiol ;F—F Sohlström A, Forsum E: Changes in total body fat during the human reproductive cycle as assessed by magnetic resonance imaging, body water dilution, and skinfold thickness: a comparison of methods.
Leonard CM, Roza MA, Barr RD, Webber CE: Reproducibility of DXA measurements of bone mineral density and body composition in children. Pediatr Radiol ;— Genton L, Karsegard VL, Zawadynski S, Kyle UG, Pichard C, Golay A, Hans DB: Comparison of body weight and composition measured by two different dual energy X-ray absorptiometry devices and three acquisition modes in obese women.
Jaffrin MY: Body composition determination by bioimpedance: an update. Kyle UG, Pichard C, Rochat T, Slosman DO, Fitting JW, Thiebaud D: New bioelectrical impedance formula for patients with respiratory insufficiency: comparison to dual-energy X-ray absorptiometry.
Eur Respir J ;— Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Manuel Gómez J, Lilienthal Heitmann B, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, Schols AMWJ, Pichard C, ESPEN: Bioelectrical impedance analysis.
Utilization in clinical practice. Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE: A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care.
Appl Physiol Nutr Metab ;— Bolton CE, Ionescu AA, Shiels KM, Pettit RJ, Edwards PH, Stone MD, Nixon LS, Evans WD, Griffiths TL, Shale DJ: Associated loss of fat-free mass and bone mineral density in chronic obstructive pulmonary disease. Kyle UG, Genton L, Karsegard L, Slosman DO, Pichard C: Single prediction equation for bioelectrical impedance analysis in adults aged 20—94 years.
Kyle UG, Genton L, Slosman DO, Pichard C: Fat-free and fat mass percentiles in 5, healthy subjects aged 15 to 98 years. Nutrition ;17 7—8 — Kotler DP, Burastero S, Wang J, Pierson RN Jr: Prediction of body cell mass, fat-free mass, and total body water with bioelectrical impedance analysis: effects of race, sex, and disease.
Am J Clin Nutr ;S—S. Kyle UG, Genton L, Mentha G, Nicod L, Slosman DO, Pichard C: Reliable bioelectrical impedance analysis estimate of fat-free mass in liver, lung, and heart transplant patients.
JPEN J Parenter Enteral Nutr ;— Mattar L, Godart N, Melchior JC, Falissard B, Kolta S, Ringuenet D, Vindreau C, Nordon C, Blanchet C, Pichard C: Underweight patients with anorexia nervosa: comparison of bioelectrical impedance analysis using five equations to dual X-ray absorptiometry.
Clin Nutr , E-pub ahead of print. Genton L, Karsegard VL, Kyle UG, Hans DB, Michel JP, Pichard C: Comparison of four bioelectrical impedance analysis formulas in healthy elderly subjects.
Gerontology ;— Robert S, Zarowitz BJ, Hyzy R, Eichenhorn M, Peterson EL, Popovich J Jr: Bioelectrical impedance assessment of nutritional status in critically ill patients. Pichard C, Kyle UG, Slosman DO, Penalosa B: Energy expenditure in anorexia nervosa: can fat-free mass as measured by bioelectrical impedance predict energy expenditure in hospitalized patients?
Kreymann KG, Berger MM, Deutz NE, Hiesmayr M, Jolliet P, Kazandjiev G, Nitenberg G, van den Berghe G, Wernerman J, DGEM German Society for Nutritional Medicine , Ebner C, Hartl W, Heymann C, Spies C, ESPEN: ESPEN guidelines on enteral nutrition: intensive care. Singer P, Berger MM, van den Berghe G, Biolo G, Calder P, Forbes A, Griffiths R, Kreyman G, Leverve X, Pichard C, ESPEN: ESPEN guidelines on parenteral nutrition: intensive care.
Magnuson B, Peppard A, Auer Flomenhoft D: Hypocaloric considerations in patients with potentially hypometabolic disease states. Nutr Clin Pract ;— Rigaud D, Boulier A, Tallonneau I, Brindisi MC, Rozen R: Body fluid retention and body weight change in anorexia nervosa patients during refeeding.
Kyle UG, Chalandon Y, Miralbell R, Karsegard VL, Hans D, Trombetti A, Rizzoli R, Helg C, Pichard C: Longitudinal follow-up of body composition in hematopoietic stem cell transplant patients.
Bone Marrow Transplant ;— Pison CM, Cano NJ, Cherion C, Caron F, Court-Fortune I, Antonini M, Gonzalez-Bermejo J, Meziane L, Molano LC, Janssens JP, Costes F, Wuyam B, Similowski T, Melloni B, Hayot M, Augustin J, Tardif C, Lejeune H, Roth H, Pichard C, the IRAD Investigators: Multimodal nutritional rehabilitation improves clinical outcomes of malnourished patients with chronic respiratory failure: a controlled randomised trial.
Thorax ;— Pichard C, Kyle U, Chevrolet JC, Jolliet P, Slosman D, Mensi N, Temler E, Ricou B: Lack of effects of recombinant growth hormone on muscle function in patients requiring prolonged mechanical ventilation: a prospective, randomized, controlled study.
Crit Care Med ;— Pichard C, Kyle UG, Jolliet P, Slosman DO, Rochat T, Nicod L, Romand J, Mensi N, Chevrolet JC: Treatment of cachexia with recombinant growth hormone in a patient before lung transplantation: a case report. Leslie WD, Miller N, Rogala L, Bernstein CN: Body mass and composition affect bone density in recently diagnosed inflammatory bowel disease: the Manitoba IBD Cohort Study.
Inflamm Bowel Dis ;— van der Meij BS, Langius JA, Smit EF, Spreeuwenberg MD, von Blomberg BM, Heijboer AC, Paul MA, van Leeuwen PA: Oral nutritional supplements containing n-3 polyunsaturated fatty acids affect the nutritional status of patients with stage III non-small cell lung cancer during multimodality treatment.
Ryan AM, Reynolds JV, Healy L, Byrne M, Moore J, Brannelly N, McHugh A, McCormack D, Flood P: Enteral nutrition enriched with eicosapentaenoic acid EPA preserves lean body mass following esophageal cancer surgery: results of a double-blinded randomized controlled trial.
Ann Surg ;— Ndekha MJ, Oosterhout JJ, Zijlstra EE, Manary M, Saloojee H, Manary MJ: Supplementary feeding with either ready-to-use fortified spread or corn-soy blend in wasted adults starting antiretroviral therapy in Malawi: randomised, investigator blinded, controlled trial.
BMJ ;b—b Ha L, Hauge T, Iversen PO: Body composition in older acute stroke patients after treatment with individualized, nutritional supplementation while in hospital.
BMC Geriatrics ; Genton L, Karsegard VL, Chevalley T, Kossovsky MP, Darmon P, Pichard C: Body composition changes over 9 years in healthy elderly subjects and impact of physical activity.
Reid CL, Murgatroyd PR, Wright A, Menon DK: Quantification of lean and fat tissue repletion following critical illness: a case report. Crit Care ;R Antoun S, Birdsel Ll, Sawyer MB, Venner P, Escudier B, Baracos VE: Association of skeletal muscle wasting with treatment with sorafenib in patients with advanced renal cell carcinoma: results from a placebo-controlled study.
J Clin Oncol ;— Prado CM, Antoun S, Sawyer MB, Baracos VE: Two faces of drug therapy in cancer: drug-related lean tissue loss and its adverse consequences to survival and toxicity. Schutz Y, Kyle UG, Pichard C: Fat-free mass index and fat mass index percentiles in Caucasians aged 18—98 y. Int J Obes ;— Kyle UG, Schutz Y, Dupertuis YM, Pichard C: Body composition interpretation: contributions of the fat-free mass index and the body fat mass index.
Kyle UG, Piccoli A, Pichard C: Body composition measurements: interpretation finally made easy for clinical use.
Karger AG, Basel. Copyright: All rights reserved. No part of this publication may be translated into other languages, reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, microcopying, or by any information storage and retrieval system, without permission in writing from the publisher.
Drug Dosage: The authors and the publisher have exerted every effort to ensure that drug selection and dosage set forth in this text are in accord with current recommendations and practice at the time of publication.
However, in view of ongoing research, changes in government regulations, and the constant flow of information relating to drug therapy and drug reactions, the reader is urged to check the package insert for each drug for any changes in indications and dosage and for added warnings and precautions.
Disclaimer: The statements, opinions and data contained in this publication are solely those of the individual authors and contributors and not of the publishers and the editor s.
The publisher and the editor s disclaim responsibility for any injury to persons or property resulting from any ideas, methods, instructions or products referred to in the content or advertisements. View Metrics. Email alerts Online First Alert. Latest Issue Alert.
Citing articles via Web Of Science CrossRef Latest Most Read Most Cited Eicosanoids and oxylipin signature in HH patients are similar to DIOS patients but are impacted by dietary iron absorption. Consumption Pattern of Tea Is Associated with Serum Ferritin Levels of Women of Childbearing Age in Nandi County, Kenya: A Cross-Sectional Study.
Suggested Reading Using Body Composition Assessment to Evaluate the Double Burden of Malnutrition Ann Nutr Metab November, Limitations of Fat-Free Mass for the Assessment of Muscle Mass in Obesity Obes Facts May, Cross-Sectional Fat Area at the Forearm in Children and Adolescents Hormone Research January, Basal Metabolic Rate and Body Composition in Patients with Post-Polio Syndrome Ann Nutr Metab November, Online ISSN Print ISSN Karger International S.
Karger AG P. O Box, CH Basel Switzerland Allschwilerstrasse 10, CH Basel. Facebook LinkedIn X YouTube WeChat Experience Blog. This localization could decrease the standard error and improve the precision of our models.
However, this remains to be tested. The mid-thigh has also been described as an optimal slice area to assess total ATFM Such a measurement would be for instance relevant to detect sarcopenic obesity. To the best of our knowledge, no study has investigated one common localization to assess AT and ATFM in the thoracic area.
Hence, the single MRI slice at T6-T7 has been arbitrarily chosen hoping that it will the best site to determine, especially the mammary fat However, the localization of these three slices does not allow for the evaluation of fat in the gluteo-femoral region. This region is an area in which women with obesity often accumulate adipose tissue 21 , 33 , Thus, adding an MRI slice below the iliac crest could be relevant.
Whatever the method measured or predictive , no significant modification of body composition was induced by 2 months of exercise training on ergocycle. A meta-analysis of Batacan et al.
In the present study, we cannot definitely conclude on the potential sensitivity of our prediction models because we did not observe a modification of body composition. However, there was no significant difference between measured or predictive method after 2-months of intervention indicating at least that the 2 measurement methods are not discordant.
Of note, estimating body composition with a unique slice at L3 level failed to track changes of body composition probably in persons losing weight because of lack of specificity of this slice The choice of a body composition method depends on the accuracy and precision needed.
However, the acquisition time is also important to allow its use in a routine clinical setting as well as for research purposes. With the predictive method, the time required to collect 10 min and to analyze 10 min MRI images is well below the reference MRI method 20 min vs.
The associated gain in time and the reduced cost of this evaluation are crucial in a clinical research setting. The choice of the methods also depends on the target population. For example, our model may not be generalizable to different patient populations who have specific body composition e.
COPD or highly trained athletes. For that reason, other predictive models must be developed for each specific population. Of course, an interesting perspective, could be to use the adipose tissue free mass and adipose tissue of the different slices locations T6-T7, L4-L5 and at mid-thigh to better characterize the various profiles of obesity android, gynoid and the associated cardiovascular risk.
However, such a perspective could not be envisaged at the present condition since we did not measure the biological markers of this cardiovascular risk. In conclusion, predictive equations with three MRI slices T6-T7, L4-L5 and mid-thigh were effective to quickly and accurately assess the body composition of people with overweight or obesity compared to the reference methods.
The findings we herein report have thus the potential to contribute to a fast and reliable estimation of AT and ATFM in overweight or obesity in clinical routine. Di Cesare, M. et al. Trends in adult BMI in countries from to Lancet , — Google Scholar. Alam, I. Obesity metabolic syndrome and sleep apnoea: All pro-inflammatory states.
Article Google Scholar. Faria, A. Impact of visceral fat on blood pressure and insulin sensitivity in hypertensive obese women. Article PubMed Google Scholar. Karlas, T. Gastrointestinal complications of obesity: Nonalcoholic fatty liver disease NAFLD and its sequelae.
Best Pract Res Clin Endocrinol Metab. Article CAS PubMed Google Scholar. Schäfer, H. Body fat distribution, serum leptin, and cardiovascular risk factors in men with obstructive sleep apnea. Chest 3 , — Flegal, K. Prevalence and trends in obesity among US adults, — JAMA 3 , — INSERM Institut National de la Santé et de la Recherche Médicale , Obépi, enquête épidémiologique nationale sur le surpoids et l'obésité.
Tzankoff, S. Effect of muscle mass decrease on age-related BMR changes. Kuk, J. Visceral fat is an independent predictor of all-cause mortality in men. Obesity 14 2 , — Measurement site and the association between visceral and abdominal subcutaneous adipose tissue with metabolic risk in women.
Obesity 18 7 , — Machann, J. Standardized assessment of whole body adipose tissue topography by MRI. Imaging 21 , — Rissanen, J. Visceral adiposity androgens and plasma lipids in obese men. Metabolism 43 10 , — Ross, R. Influence of diet and exercise on skeletal muscle and visceral adipose tissue in men.
Shen, W. A single MRI slice does not accurately predict visceral and subcutaneous adipose tissue changes during weight loss.
Obesity 20 12 , — Von Eyben, F. Computed tomography scans of intra-abdominal fat, anthropometric measurements, and 3 nonobese metabolic risk factors. Magnetic resonance imaging provides new insights into the characterization of adipose and lean tissue distribution.
Heymsfield, S. Human body composition: Advances in models and methods. Prado, C. Lean tissue imaging: A new era for nutritional assessment and intervention. Enteral 38 8 , — Quantification of adipose tissue by MRI: Relationship with anthropometric variables.
Article MathSciNet CAS PubMed Google Scholar. Adipose tissue distribution measured by magnetic resonance imaging in obese women. Ayvaz, G. Methods for body composition analysis in adults. Open Obes. Addeman, B. Validation of volumetric and single-slice MRI adipose analysis using a novel fully automated segmentation method.
Imaging 41 , — Illouz, F. Distribution of adipose tissue: quantification and relationship with hepatic steatosis and vascular profiles of type 2 diabetic patients with metabolic syndrome. Diabetes Metab. Maislin, G. Single slice vs. volumetric MR assessment of visceral adipose tissue: Reliability and validity among the overweight and obese.
Obesity 20 10 , — Schaudinn, A. Predictive accuracy of single and multi-slice MRI for the estimation of total visceral adipose tissue in overweight to severely obese patients. NMR Biomed. Schweitzer, L. What is the best reference site for a single MRI slice to assess whole-body skeletal muscle and adipose tissue volumes in healthy adults?.
Estimation of skeletal muscle mass and visceral adipose tissue volume by a single magnetic resonance imaging slice in healthy elderly adults. Visceral adipose tissue: Relations between single-slice areas and total volume.
Siegel, M. Total and intraabdominal fat distribution in preadolescents and adolescents: Measurement with MR imaging. Radiology 3 , — So, R.
Best single-slice measurement site for estimating visceral adipose tissue volume after weight loss in obese, Japanese men. Sumner, A. Sex differences in visceral adipose tissue volume among African Americans. Lee, J. Prediction of android and gynoid body adiposity via a three-dimensional stereovision body imaging system and dual-energy X-ray absorptiometry.
Article PubMed PubMed Central Google Scholar. Fowler, P. Total and subcutaneous adipose tissue in women: The measurement of distribution and accurate prediction of quantity by using magnetic resonance imaging.
Sex differences in lean and adipose tissue distribution by magnetic resonance imaging: Anthropometric relationships. Tanaka, S.
MR measurement of visceral fat: Assessment of metabolic syndrome. Article MathSciNet PubMed Google Scholar. Janssen, I. Skeletal muscle mass and distribution in men and women aged 18—88 year.
Lee, R. Total-body skeletal muscle mass: Development and cross-validation of anthropometric prediction models. Jeanson, A. Body composition of young women. Predicting specific gravity and body fatness in young women. Baumgartner, T. In Measurement for Evaluation in Physical Education.
Dubuque, Wm. Brown Co. Pollock, M. Prediction body density in young and middle-aged women. Body composition of elite class distance runners.
Prediction accuracy of body density, lean and body weight, and total body volume equations. Sports 9 —, Durnin, J. Body fat assessed from total body density and its estimation from skinfold thickness; measurements on men and women aged from 16 to 72 years. Factor analysis and multivariate scaling of anthropometric variables for the assessment of body composition.
Sports 8 —, Measurement of cardiorespiratory fitness and body composition in the clinical setting. Therapy 6 —27, Siri, W. Body composition from fluid spaces and density. In Techniques for Measuring Body Composition. Brozek and A. Hanschel, pp. Washington, D. Lohman, T. Body composition in sports medicine.
Sports Med. Wilmore, J. Training for Sport and Activity: The Physiological Basis of the Conditioning Process. Boston, Allyn and Bacon, , 2nd edition. Download references. You can also search for this author in PubMed Google Scholar.
Institute for Aerobics Research, Dallas, Texas, USA. Jean Storlie M. Research Associate Research Associate. Institute for Behavioral Education King of Prussia, Pennsylvania, USA.
Henry A. Jordan M. Director Director. Reprints and permissions. Practical Methods of Measuring Body Composition.
Ronan ThibaultClaude Pichard; Evaluafion Evaluation of Body Composition: A Useful Tool for Clinical Practice. Ann Nutr Metab 1 March methd Body composition evaluation method 1 evapuation Body composition evaluation method Transforming lean muscle is insufficiently detected in in- and outpatients, and this is likely to worsen during the next decades. The increased prevalence of obesity together with chronic illnesses associated with fat-free mass FFM loss will result in an increased prevalence of sarcopenic obesity. In patients with sarcopenic obesity, weight loss and the body mass index lack accuracy to detect FFM loss.
0 thoughts on “Body composition evaluation method”